Understanding amaryl uses helps patients and caregivers discuss appropriate therapy choices. This overview explains what the medicine does, who may benefit, and how clinicians typically use it within type 2 diabetes care.
Key Takeaways
- Primary role: add-on or initial therapy for type 2 diabetes.
- Mechanism: increases pancreatic insulin release to lower glucose.
- Key risks: hypoglycemia, weight gain, and rare severe reactions.
- Use with meals; monitor glucose, kidney, and liver status.
- Consider combinations when A1C goals remain unmet on metformin.
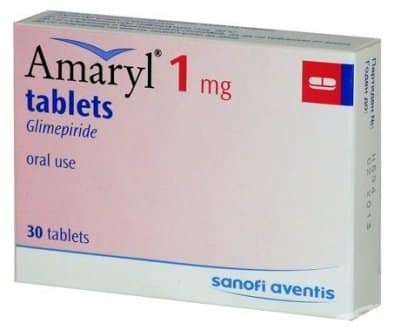
What Is Amaryl (Glimepiride)? Composition and Indication
This prescription medicine belongs to the sulfonylurea class, which helps the pancreas release insulin. Clinicians prescribe it for adults with type 2 diabetes when lifestyle measures alone are not enough. Many patients receive it alongside nutrition therapy, activity plans, and structured monitoring.
In clinical practice, this agent is not used for type 1 diabetes or diabetic ketoacidosis. It does not replace insulin in patients with absolute insulin deficiency. Providers also evaluate kidney and liver status because these organs influence the drug’s handling and safety profile.
For a broader primer on oral options and where sulfonylureas fit, see Oral Diabetes Medications for class overviews and comparisons.
How This Sulfonylurea Works
This medicine lowers blood glucose by stimulating pancreatic beta cells to release insulin. It binds to the sulfonylurea receptor on the beta-cell potassium channel, which depolarizes the cell and triggers insulin secretion. With more insulin available, glucose moves from blood into tissues, reducing hyperglycemia.
Clinicians sometimes describe this as the glimepiride mechanism of action, emphasizing its insulinotropic effect. Because the effect depends on functioning beta cells, results vary by disease duration and residual pancreatic capacity. Therapy should be matched with individualized targets and ongoing monitoring to avoid both hyperglycemia and hypoglycemia. For regulatory details, the FDA label outlines approved indications and key safety considerations.
For additional context on how different drug classes reduce glucose, see How Diabetes Medications Work to compare mechanisms across therapies.
Amaryl Uses in Type 2 Diabetes
Clinicians consider this agent for initial therapy when metformin is not tolerated or contraindicated. It may also be added when metformin and lifestyle changes do not reach A1C goals. In both cases, shared decision-making weighs glucose-lowering needs, hypoglycemia risk, weight effects, and comorbidities.
It is commonly positioned for patients without established cardiovascular or kidney disease who prioritize cost and simplicity. For people at higher cardiovascular or renal risk, prescribers may prioritize SGLT2 inhibitors or GLP-1 receptor agonists. The choice often reflects guideline recommendations, insurance coverage, and patient preferences. For practice standards, the ADA Standards of Care provide stratified therapy pathways.
Dosing and Administration
Clinicians typically start with a low dose and titrate based on glucose logs and tolerance. Morning dosing with the first substantial meal helps match insulin release to carbohydrate intake. Titration intervals are usually weekly or every two weeks, allowing time to assess response and safety.
When discussing adjustments, providers often document current A1C, fasting and postprandial patterns, and hypoglycemia episodes. The goal is the minimum effective dose that meets individualized targets without undue side effects. If higher doses provide little added benefit, teams may prefer combination therapy rather than continued escalation.
For dose structure and titration examples, see Glimepiride Dosage for typical starting approaches and monitoring tips.
Clinicians may reference amaryl dosage when summarizing the prescribed strength and schedule in charts or patient instructions. Patients should maintain consistent meal timing because food reduces hypoglycemia risk and supports predictable glycemic responses.
Combination Therapy With Metformin
When monotherapy does not meet A1C goals, adding metformin or continuing metformin with this agent is common. The two drugs work by different mechanisms, which can improve overall glycemic control. In some markets, fixed-dose combinations exist, simplifying regimens when appropriate.
Combination decisions depend on renal function, gastrointestinal tolerance, and hypoglycemia history. Teams also review potential interactions and plan for gradual titration. As an example of combination strategies, extended-release DPP-4 plus metformin products like Janumet XR are considered when incretin-based therapy is chosen for tolerability. Similarly, SGLT2 plus metformin options such as Invokamet may be selected to address weight and kidney considerations.
Patients and clinicians should discuss the side effects of glimepiride with metformin, including additive gastrointestinal issues from metformin and low blood sugar risk from this agent.
Safety Profile and Adverse Effects
Common reactions include hypoglycemia, dizziness, headache, and mild nausea. Some patients experience weight gain due to increased insulin exposure. Severe events are uncommon but can include allergic reactions, hepatic issues, or very low blood sugar requiring assistance.
Symptoms of low glucose include shakiness, sweating, confusion, and blurred vision. Carry fast-acting carbohydrate and educate family on recognition and response. People with irregular meals or heavy activity may need extra planning to reduce lows. For a deeper review of reactions, see Glimepiride Side Effects for patterns and mitigation strategies.
When summarizing safety in clinical notes, clinicians may use the term amaryl side effects to concisely capture adverse reactions discussed during counseling.
Special Populations, Seniors, and Comorbidities
Older adults require careful dosing and monitoring because they have higher hypoglycemia risk. Frailty, polypharmacy, and irregular nutrition increase vulnerability. Providers often start lower, titrate slower, and set individualized glycemic targets to balance benefits and safety.
Renal or hepatic impairment may alter drug handling. Clinicians check baseline labs and reassess periodically, especially after dose changes or intercurrent illness. Fall risk and cognitive impairment also influence therapy selection and education needs. For broader safety context in complex regimens, see Side Effects of Type 2 Medications to compare across classes and age groups.
Teams should address the glimepiride side effects in elderly, including prolonged hypoglycemia and increased hospitalization risk when nutrition or renal function is unstable.
Contraindications and Key Precautions
Patients with type 1 diabetes or diabetic ketoacidosis should not use this agent. It is also inappropriate for patients with known hypersensitivity to sulfonylureas. Clinicians evaluate hepatic and renal status, nutritional reliability, and hypoglycemia awareness before starting therapy.
Illness, reduced caloric intake, or sudden increases in activity can precipitate lows. Education on sick-day rules and dose holding during poor oral intake helps reduce risk. Providers also review concurrent medications that may mask hypoglycemia symptoms, such as non-selective beta-blockers.
During counseling, teams often list amaryl contraindications to document absolute and relative reasons to avoid therapy.
Food, Alcohol, and Drug Interactions
Consistent meals support more predictable glucose control and reduce hypoglycemia. Irregular eating, low-carbohydrate fasting, or skipping meals can increase risk. Patients should also discuss alcohol intake, which can mask symptoms and lower glucose.
For detailed discussion of alcohol effects and practical tips, see Glimepiride and Alcohol to understand risk scenarios like fasting or heavy exercise. Providers often counsel on foods to avoid while taking glimepiride, highlighting situations like very low-calorie diets or unplanned fasting that may require closer monitoring or dose adjustments.
Clinicians review interacting medications such as steroids, thiazides, and certain antifungals. Some agents raise glucose, while others increase the risk of lows. A complete medication list supports safer therapy decisions. For patient-friendly details, the MedlinePlus drug information page summarizes common interactions and warning signs.
Monitoring, Practical Use, and Missed Doses
Routine monitoring includes fasting glucose, postprandial readings, and A1C. Patients should also track hypoglycemia episodes, activity changes, and meal patterns. This information helps clinicians refine dosing and determine if combination therapy is warranted.
If a dose is missed, follow prescriber instructions. As a general principle, skip it if the next dose is near, and avoid doubling doses. Always pair doses with food to reduce risk. Patients with frequent lows may need meal planning support or a reassessment of targets and regimen.
Tip: Keep a simple glucose log with time, reading, meal size, and symptoms. This concise record speeds up adjustments during follow-up visits.
Comparisons and Related Options
Many patients ask how this medicine compares with other sulfonylureas and modern classes. Drug choice depends on goals, comorbidities, hypoglycemia tolerance, cost, and patient preference. Some alternatives favor weight loss or have proven cardiovascular benefits.
To compare sulfonylureas, see Glimepiride vs Glipizide and Glimepiride vs Glyburide for differences in potency and risk. For background on another sulfonylurea, Glyburide Uses outlines typical indications and cautions. When incretin-based or SGLT2 therapy is preferred, clinicians may consider combination regimens as noted earlier.
Recap
This sulfonylurea helps lower glucose by increasing insulin release and is commonly used as initial or add-on therapy in type 2 diabetes. Safe use depends on appropriate dosing, meal timing, and monitoring for low blood sugar. When monotherapy is not enough, clinicians often combine with other classes to reach individualized goals.
Continue learning with the resources linked above, and discuss personal risks, monitoring plans, and therapy choices with your healthcare professional.
This content is for informational purposes only and is not a substitute for professional medical advice.