Key Takeaways
- Unified targets: align blood pressure, glucose, and lipids to reduce risk.
- Layered care: combine lifestyle, nutrition, and evidence-based medications when needed.
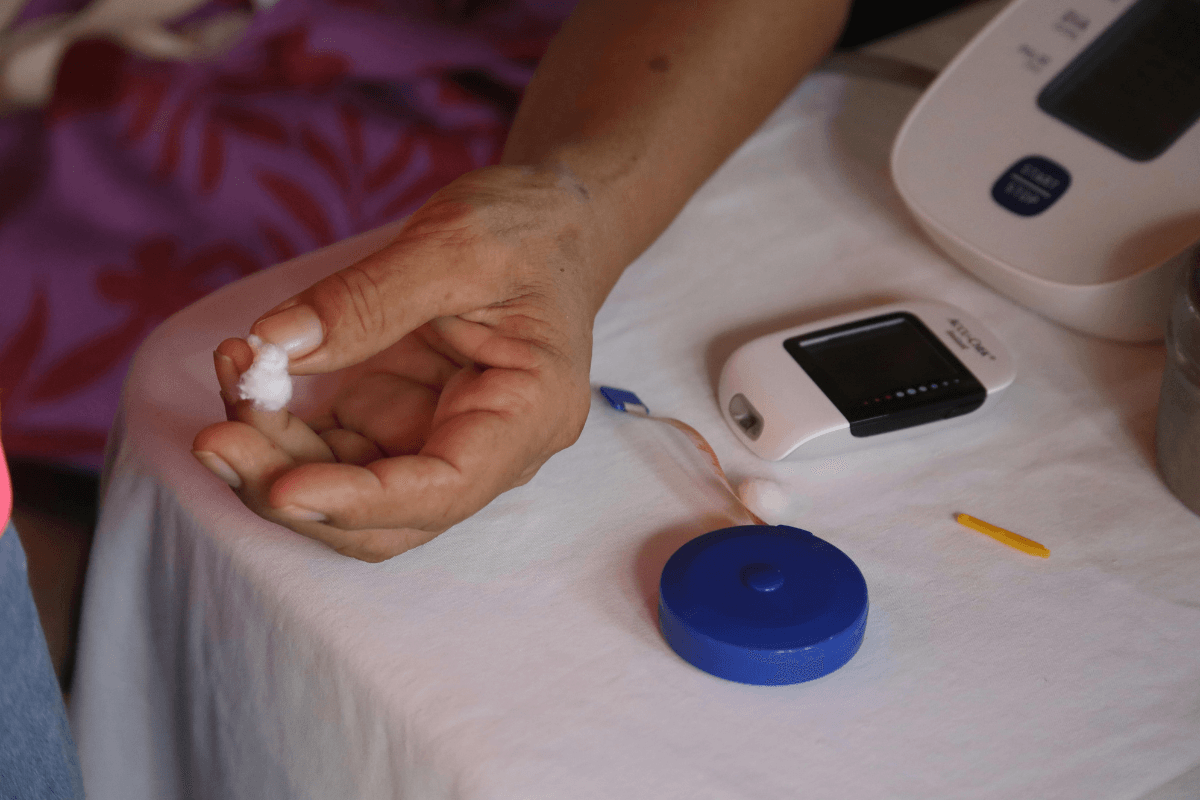
- Home monitoring: track readings, symptoms, and side effects in one log.
- Risk focus: protect kidneys, eyes, nerves, and the heart proactively.
Understanding the Overlap: Pathways and Risks
Many adults live with diabetes and hypertension, and the overlap raises cardiovascular and kidney risk. Insulin resistance, chronic inflammation, and arterial stiffness interact. Over time, small vessels in the kidneys and eyes become vulnerable. Early detection and steady control help limit long-term complications.
Glucose variability can worsen vascular tone, while elevated pressure accelerates endothelial injury. That two-way stress may increase atherosclerosis risk. For context on population burden and prevention basics, see the Centers for Disease Control and Prevention overview of hypertension for definitions and trends. When kidneys are affected, albumin in the urine often rises first; for a deeper primer on kidney damage mechanisms, see Diabetic Nephropathy Overview to understand early warning signs.
Diabetes and Hypertension: Why the Link Matters
Shared risk factors include weight gain, sedentary routines, and family history. Sleep apnea, high sodium intake, and certain medicines can also push readings higher. Addressing these drivers together usually improves outcomes more than treating either condition alone.
Cardiovascular events remain the main threat. Small improvements across several numbers often beat large changes in one. This is why care plans commonly align blood pressure goals with individualized glucose and lipid targets. Team coordination reduces conflicting advice and minimizes treatment burden.
Targets and Monitoring: Blood Pressure, Glucose, and Lipids
Most adults aim for practical thresholds individualized to comorbidities and tolerance. For many, hitting a normal blood pressure range reduces stroke and kidney risks. Discuss specific thresholds with your clinician, especially if you have coronary disease, pregnancy, or autonomic neuropathy. The American Diabetes Association updates annual guidance; see the ADA Standards of Care for target ranges and monitoring suggestions.
Home monitoring catches trends earlier than clinic checks. Take morning and evening seated readings, and record context like caffeine, exercise, and stress. Use the same validated cuff and proper fit. For diagnostic categories and treatment thresholds, refer to the ACC/AHA guideline for standardized definitions and staging. Pair blood pressure logs with fasting glucose and periodic A1C to see patterns.
Nutrition Strategy: Practical Eating for Dual Control
Food choices influence insulin sensitivity, volume status, and vascular health. Focus on vegetables, legumes, lean proteins, nuts, and whole grains. Limit sodium to a personalized threshold, often supported by label reading and cooking at home. People often ask what should a diabetic with high blood pressure eat. In practice, steady fiber intake, potassium-rich foods, and modest portions of low-fat dairy can support both conditions.
Build a flexible plan. Use culturally familiar ingredients and simple swaps, like herbs for salt or olive oil for butter. Consider a structured weekly plan to reduce decision fatigue. If you need an organized starting point, adapt a balanced template rather than depending on a rigid diabetic diet food list, and keep hydration consistent across the day.
Medications: Classes, Combinations, and Safety
Medicine choices depend on age, kidney function, pregnancy status, and comorbidities. Angiotensin pathway blockers, thiazide diuretics, and calcium channel blockers are frequently used. Clinicians often consider ace inhibitors for hypertension and diabetes because they may protect kidneys in albuminuria. If cough occurs with an ACE inhibitor, an ARB may be an alternative.
First-Line Choices and Add-Ons
ARBs are common when ACE inhibitors are not tolerated. For example, Valsartan is frequently chosen in metabolic syndrome; review it for an ARB example. Thiazide-type diuretics lower volume and vascular resistance; for thiazide details and typical use cases, see Hydrochlorothiazide. Dihydropyridine calcium channel blockers help when vasodilation is needed; see Nifedipine for a commonly used agent. Another ARB option is Telmisartan, which is sometimes selected for patients with metabolic concerns.
Medication selection requires periodic review of electrolytes, creatinine, and symptoms like dizziness or edema. Discuss interactions with glucose-lowering drugs and diuretics. For additional context on ACE inhibitor therapy, see Altace and Blood Pressure for a brand-focused overview of clinical use cases.
When Combination Therapy Helps
Two drugs may be used when a single agent does not reach targets. A low-dose pairing can minimize side effects while improving control. Combination tablets can also improve adherence by reducing pill burden. If your clinician recommends an ACE inhibitor plus thiazide, see Ramipril HCTZ for a typical combination option. Adjustments should follow several weeks of home readings and lab checks, especially if diuretics affect potassium or kidney function.
Lifestyle and Exercise: Daily Habits That Move Numbers
Small habits add up. Brisk walking, strength training, and sleep hygiene each influence vascular tone and insulin action. If you want guidance on how to lower blood pressure, begin with 150 minutes weekly of moderate activity and two days of resistance work, as tolerated. Add short movement breaks during long sitting periods.
Limit alcohol, stop tobacco, and address sleep apnea when suspected. Track sodium from packaged foods and restaurant meals. Restorative sleep helps hormone balance and appetite control. If dizziness or lightheadedness occurs, review your plan; see Low Blood Pressure and Diabetes for a discussion of hypotension risks and warning signs.
Complications and Risk Reduction
The combination of type 2 diabetes and hypertension raises cardiovascular and renal risk. Retinopathy and neuropathy also become more likely with prolonged exposure to high glucose and pressure. Regular eye exams, urine albumin tests, and foot checks detect changes early. Statin therapy is frequently considered for lipid control in high-risk adults.
Some glucose-lowering medications offer cardiovascular benefits. For a review of protective effects beyond glycemia, see Metformin Cardioprotective Effects for mechanism summaries. Kidney protection starts with consistent monitoring and prompt treatment adjustments. Comprehensive, steady control beats intermittent, aggressive changes.
Care Plan and Follow-Up: Build a Sustainable Routine
Set up a shared care plan with clear targets, including blood pressure for diabetics type 2 tailored to your risks. Use a single log for blood pressure, glucose, weight, activity, and notable symptoms. Bring the log to visits so your clinician can adjust therapy based on trends and side effects. Schedule labs at recommended intervals, including potassium and creatinine when on diuretics or renin-angiotensin blockers.
Education reduces uncertainty and improves adherence. Explore related topics to learn the rationale behind drug choices and monitoring. For broader heart and vessel topics that intersect with metabolic care, see our Cardiovascular Articles for context on risk management. When medicines are reviewed, ask about timing, interactions, and what to watch for between visits.
Recap
Coordinated care across nutrition, activity, and medications helps reduce long-term risk. Use home monitoring to guide steady, small adjustments. Personalize targets with your clinician, and protect the heart, kidneys, eyes, and nerves through consistent follow-up. Focus on progress you can sustain.
This content is for informational purposes only and is not a substitute for professional medical advice.