Combination insulin options can simplify daily injections and meal coverage. Used correctly, premixed insulin may streamline routines while balancing blood glucose before and after meals. This guide summarizes how mixes work, common ratios, timing, safety, and where they fit compared with flexible basal–bolus plans.
Key Takeaways
Many adults prefer premixed insulin for fewer daily injections and straightforward timing. Premixed insulin combines intermediate and rapid/short components to cover fasting and meal-related needs.
- Two-in-one action: One injection covers basal background and mealtime spikes.
- Predictable routine: Fixed ratios encourage consistent meal timing and portions.
- Fewer injections: Usually one to two doses per day versus multiple boluses.
- Less flexibility: Harder to adjust doses for unexpected meals or exercise.
- Safety first: Monitor for hypoglycemia (low blood sugar) and weight gain.
What Is Premixed Insulin?
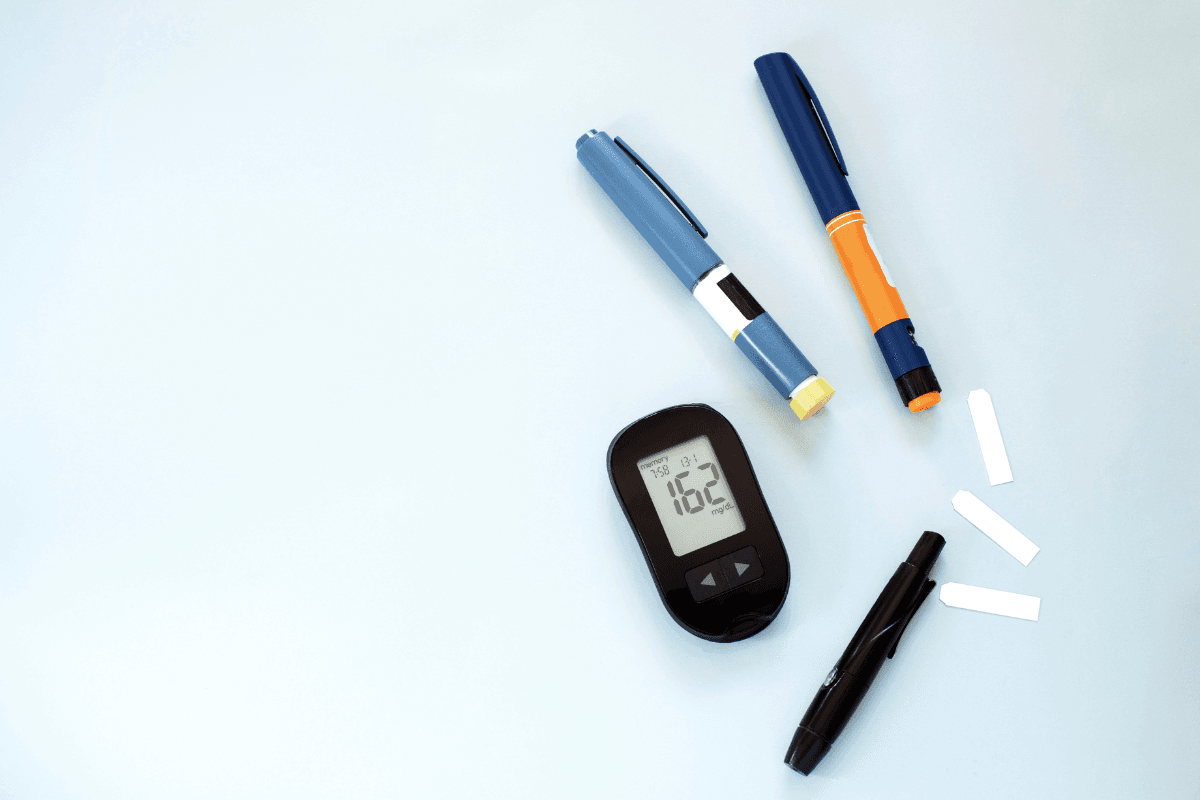
These products blend two insulin actions in a single pen or vial: a rapid- or short-acting prandial component (mealtime insulin) and an intermediate-acting basal component (background insulin). The fixed ratio aims to manage both fasting and post-meal glucose with fewer decisions. Compared with assembling separate basal and bolus doses, mixes can reduce complexity for people who value routine.
Common human mixes combine regular insulin with NPH (neutral protamine Hagedorn). Analog mixes pair rapid-acting analogs with protamine-crystallized versions of the same analog. Each ratio dictates how much of the dose targets mealtime spikes versus all-day coverage. Because the ratio is fixed, patients and clinicians often anchor dosing to stable meal timing and consistent carbohydrate intake.
Mechanism of Action and Combinations
Mixes deliver a biphasic profile: a rapid early peak for meals and a slower second phase for background control. The early component reduces postprandial excursions, while the intermediate component supports between-meal and overnight needs. This dual action may reduce glycemic variability (glucose swings) when meals and activity are predictable. However, when meals are delayed or missed, the prandial portion can increase hypoglycemia risk.
Analog options, including biphasic insulin aspart 30, typically act faster before meals than human 70/30 products. Human mixes may need earlier pre-meal administration to match absorption. Product-specific pharmacokinetics vary by formulation and ratio. For detailed therapy standards, see the ADA Standards of Care (ADA Standards of Care), and for Canadian practice guidance, review Diabetes Canada recommendations (Diabetes Canada guidelines).
Types and Brands
Human mixes commonly appear as 30/70 or 50/50 ratios, while analog mixes often include 70/30 or 75/25 ratios. Each describes the percentage of rapid/short action versus intermediate action. When comparing types of premixed insulin, consider onset time, peak effect, and duration alongside your meal schedule. Analog mixes usually allow closer-to-meal dosing, while human mixes often need a longer lead time.
Examples include 30/70 human formulations and analog combinations such as 75/25 and 50/50. Specific brands vary by region and device format. For a brand example of human 30/70, see Novolin GE 30/70 Vials for typical composition details. Another human 30/70 option is illustrated by Humulin 30/70 Vial, useful when comparing vial-based regimens. For an overview of a related delivery device, this article on Humalog Mix Kwikpen Guide explains how prefilled pens can streamline daily use.
Note: Brand names and device formats differ by market. Always verify product strength, ratio, and device compatibility before switching devices or formulations.
Dosing Schedules and Timing
Dosing plans center on consistent meals, portion sizes, and activity. A typical premixed insulin dosing schedule uses once- or twice-daily injections aligned with breakfast and the evening meal. Human 30/70 mixes are often given earlier before meals, while analog mixes may be timed closer to eating. Your prescriber tailors timing and dose based on glucose logs, nutrition, and risk factors.
Administration timing reflects the formulation. Human regular/NPH mixes often require dosing 20–30 minutes before eating. Analog mixes are frequently dosed immediately before meals. For device and formulation differences, see Short-Acting Insulin for prandial timing context, and review Intermediate-Acting Insulin Types for background coverage characteristics. For safe storage thresholds and stability guidance, consult Insulin Storage 101.
Tip: Align dosing and meal timing with your specific formulation. Adjusting meal timing without dose review can increase hypoglycemia risk.
Initiation and Titration Basics
Starting therapy typically involves once-daily or twice-daily dosing, then careful adjustments over several weeks. A structured premixed insulin titration algorithm often uses fasting and pre-supper glucose targets to guide small stepwise changes. Clinicians consider patterns, not isolated values, and weigh hypoglycemia episodes before increasing doses. Safe titration depends on accurate logging, consistent meals, and recognition of low-glucose symptoms.
When initiating, clinicians may choose an evening or breakfast anchor based on lifestyle and predominant hyperglycemia patterns. Education covers injection technique, rotation, and recognizing lows. For cartridge and pen format considerations, see Insulin Cartridges Types to compare device pros and cons. Clinical protocols differ by region; consult local guidance and product monographs for timing, mixing restrictions, and maximum single-injection volumes (Diabetes Canada guidelines).
Comparing Mixes With Basal–Bolus Plans
Premixed regimens simplify therapy by reducing daily decisions and injection counts. However, premixed insulin vs basal-bolus reveals trade-offs. Basal–bolus allows independent adjustments for basal needs, meal size, and corrections. Mixes tie basal and bolus together, which can limit flexibility during variable schedules, irregular meals, or unplanned exercise.
People with consistent routines may achieve similar A1C with mixes, though hypoglycemia patterns can differ. Those who need frequent corrections, variable carbohydrates, or flexible meal timing may prefer basal–bolus. For a broader overview of insulin types and timing, see Types Insulin Onset Peak, and for strategy contrasts, review Basal vs Bolus Insulin.
Safety, Side Effects, and Education
Common concerns include hypoglycemia, weight gain, and injection site reactions. A focus on premixed insulin side effects highlights the importance of meal consistency and self-monitoring. Skipped meals, extra activity, alcohol, or dose errors can trigger lows. Carry rapid-acting carbohydrates, recognize warning signs, and review patterns with a clinician when lows occur.
Rotate injection sites to reduce lipohypertrophy (fatty tissue buildup) and absorption variability. Verify device priming, needle changes, and dose visibility before each injection. For safe handling, this article on Dangers of Improper Insulin Storage explains how temperature excursions can reduce potency. For authoritative safety information, product labeling provides detailed adverse reaction profiles and timing instructions (FDA labeling database).
Special Populations and Clinical Fit
In type 2 diabetes, mixes may suit people seeking fewer injections and predictable meals. They can be used when oral agents are insufficient or when basal alone no longer achieves targets. In type 1 diabetes, premixed insulin type 1 diabetes regimens may be considered only in select situations. Most guidelines favor flexible basal–bolus because it separates background and mealtime needs for finer control.
Shift workers, unpredictable eaters, and those needing frequent corrections may struggle with fixed ratios. Conversely, individuals with consistent schedules may find mixes manageable and effective. For education tailored to diagnosis, explore the Type 1 Diabetes and Type 2 Diabetes categories, which group related therapy articles by condition.
Examples and Ratios in Practice
Real-world use often centers on 70/30 and 75/25 analog mixes and 30/70 human mixes. People eating three structured meals may use morning and evening doses that bracket the workday. Some plans add a midday dose when lunchtime is large and regular. Devices vary; vials and syringes allow traditional dosing, while pens may offer finer increments and convenience.
To understand how a specific analog mix pen works in daily life, see Innovations in Insulin Delivery for device evolution context. If you prefer prefilled pens with integrated mixes, the Humalog Mix Kwikpens page illustrates a device format and ratio presentation without clinical endorsement.
Education Checklist for Daily Use
Daily success relies on practical habits. Keep timing consistent, match carbohydrate intake to your usual portions, and log pre- and post-meal readings. Understand sick-day rules and when to contact your care team about unexpected highs or repeated lows. Ensure backup supplies, including needles, sensors or meters, and rapid-acting carbohydrates.
Refresh your technique periodically with a nurse educator or pharmacist. Confirm expiration dates and look for solution changes or clumping in suspension products before use. If your plan changes or you switch formulations, review differences in onset, peak, and timing. For human and analog distinctions, compare Intermediate-Acting Insulin and prandial references above for context.
Recap
Premixed combinations deliver meal and background coverage in one injection. They favor people with structured routines and steady meals. Fixed ratios can simplify decisions but restrict flexibility compared with fully adjustable basal–bolus therapy. Safe timing, education, and steady nutrition patterns are central to consistent results.
Work with your clinician to determine whether a mix, basal–bolus, or another approach fits your goals, lifestyle, and safety profile. Small, methodical adjustments usually work better than sweeping changes. Track patterns, prevent lows, and use device features that support your routine.
This content is for informational purposes only and is not a substitute for professional medical advice.