Key Takeaways
- Heat, freezing, and light degrade insulin and reduce potency.
- Time out of refrigeration matters; track hours and temperatures.
- Visual changes, clumping, or frothing may indicate compromised insulin.
- After opening, follow product-specific room temperature limits carefully.
- Use reliable cooling strategies during travel and daily carry.
Small mistakes with insulin storage can lead to less effective doses and unpredictable glucose control. Many failures happen silently, such as brief overheating or accidental freezing. Addressing these risks early protects dose consistency and safety.
Insulin Storage: What Goes Wrong and Why
Insulin is a protein solution that loses activity when exposed to heat, freezing, or direct light. Repeated temperature swings strain molecular structure, which may lower potency over time. Freezing destroys the formulation immediately, while overheating accelerates degradation. Shaking some insulin types vigorously can also create bubbles and foam that suggest damage.
Manufacturers specify storage ranges and in-use durations to protect stability. These limits are conservative, but they assume correct handling from factory to patient. For authoritative guidance on general handling, see the ADA recommendations on insulin storage (ADA recommendations). For product-specific instructions, consult the manufacturer label, such as the Humalog label for storage times and temperatures (Humalog label). For foundational steps and a plain-language overview, see Insulin Storage 101 for baseline best practices on this site (for fundamentals, see Insulin Storage 101).
Temperature Limits and Stability Windows
Most insulin products are transported refrigerated, then used at room temperature according to label-specific windows. Heat speeds breakdown, while freezing causes irreversible denaturation. The usable window varies by brand and formulation, but the core idea remains the same: keep your insulin within the labeled temperature range and discard it when the in-use clock expires. If a dose seems less effective after a heat event, contact your care team before making changes.
People often ask how long can insulin be unrefrigerated. The answer depends on formulation and approved in-use durations, which are stated on the carton and package insert. Short-acting analogs, long-acting basals, and premixed options can have different room-temperature lifespans. To avoid confusion, write the first-use date on the pen or vial. A small thermometer in a bag or case helps verify daily conditions during commutes and workdays.
Signs Your Insulin Is Compromised
Visual inspection can reveal some, but not all, problems. Clear rapid-acting insulin should remain transparent and colorless, without haze, flakes, or strings. For suspensions that are supposed to look cloudy, a gentle roll should disperse crystals evenly. Persistent clumps, froth, or particles suggest degradation or contamination.
Changes in glucose patterns may also signal potency loss from heat or freezing. If correction doses seem ineffective, consider whether storage conditions slipped. For a deeper look at what appearance changes mean, see our article What Is Cloudy Insulin for practical examples and caution signs (for appearance cues, see What Is Cloudy Insulin).
Two Hours at Room Temperature
It’s common to worry about insulin left out of fridge for 2 hours. Two hours at typical indoor room temperature often falls within many products’ in-use allowance, but only if the pen or vial is otherwise in good condition and within its labeled window. Actual temperature matters more than the clock; 30°C (86°F) air warms a cartridge faster than 20°C (68°F).
Document the time, note the conditions, and monitor for expected glucose response. If the insulin was exposed to a hot car, radiator, or sunny windowsill, treat the risk as higher. For more background on daily care and prevention strategies, browse our Type 1 Diabetes section, which covers practical routines for consistent handling (for broader context, see Type 1 Diabetes).
Twenty-Four Hours or More
Concerns increase markedly with insulin left out of fridge for 24 hours, especially if temperatures are elevated. Many labels permit room-temperature storage only during a defined in-use period, and higher ambient heat shortens real-world safety margins. Unreliable cooling at work, school, or during travel can compound the risk. When in doubt, consider replacing questionable insulin instead of risking poor glycemic control.
Storage rules also vary across products. For instance, different rapid analogs and basal formulations have distinct in-use durations and temperature caps. If you want to compare label differences before adjusting routines, see our brand overview pages Humulin vs. Humalog for general distinctions and how they affect handling (for label contrasts, see Humulin vs. Humalog) and Tresiba vs. Lantus for basal-specific considerations (for basal comparisons, see Tresiba vs. Lantus).
After Opening: Pens, Vials, and Cartridges
Once opened, products move onto an in-use clock that governs room-temperature duration. This practical period differs by brand and device, so always confirm dates on the carton and insert. Labeling also specifies whether to discard after a fixed number of days, regardless of remaining volume. To simplify tracking, write the start date directly on the pen or vial with a fine marker.
Understanding device specifics reduces accidental waste. For example, pen cartridges and multi-dose vials may share similar stability windows but have different handling steps. If you use cartridges, review correct handling and replacement basics in our Insulin Cartridges Guide, which explains device types and safety cues (for cartridge handling, see Insulin Cartridges Guide). Remember that insulin storage after opening policies are based on maintaining stable room temperature and avoiding heat spikes.
Refrigerate After Opening?
Labels vary on whether opened pens and vials should remain at room temperature or return to the refrigerator. The decision hinges on the product’s instructions and your environment. Some pen devices are designed to be kept at room temperature during use to promote consistent dosing comfort, while others can be refrigerated between doses if that suits your routine. Sudden temperature swings, however, are best avoided.
Always follow the product insert for exact guidance. If ambient conditions run hot, consider a small cooler during the day even when the label allows room temperature. This reduces thermal stress and helps preserve potency. When asking should insulin be refrigerated after opening, let the specific brand guidance, local climate, and daily patterns be your primary guides.
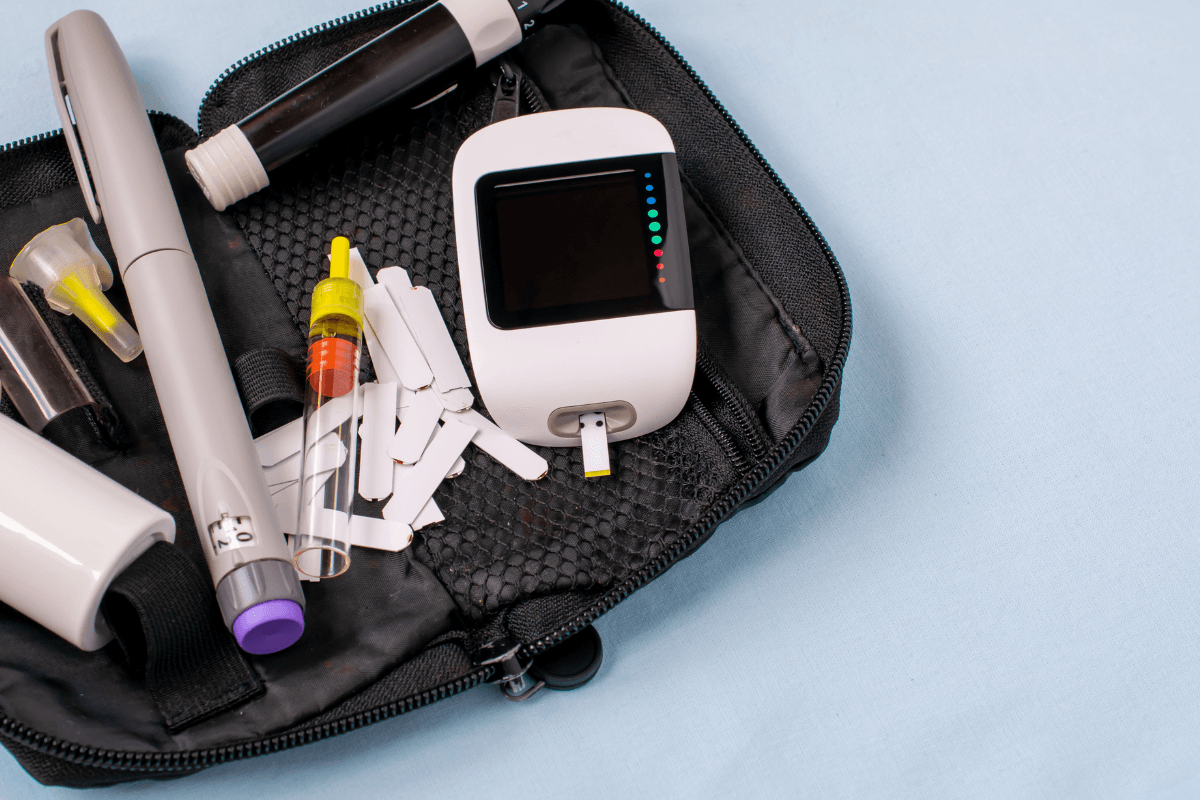
Travel and TSA Considerations
Airports, cars, and hotel rooms introduce new storage challenges. Use a thermometer-enabled case and cooling packs designed for medications. Soft-sided cases protect against temperature spikes and light while fitting into day bags. For airport screening, pack supplies in your carry-on and keep prescriptions handy. If you fly often, a tsa approved insulin travel case can simplify security checks and maintain safer temperatures in transit.
Plan for backup insulin and redundancy in cooling. Keep medications out of checked baggage to avoid extreme temperatures and loss risk. For packing steps and screening tips, see Traveling With Diabetes, which outlines preparation and in-transit safeguards (for travel planning, see Traveling With Diabetes). To reduce breakage risk when moving vials through crowded airports, a Vial Safe Insulin Protector adds impact protection without adding bulk (for impact protection, see Vial Safe Insulin Protector). If you use cartridges on the road, our Lantus Insulin Cartridge page covers device specifics relevant to packing and handling (for device context, see Lantus Insulin Cartridge).
How to Think About Unrefrigerated Time
Time out of the fridge does not automatically ruin insulin; context is everything. Room temperature varies by location, season, and micro-environments like cars and window ledges. Tracking conditions provides better insight than guessing. Note the start time, location, and approximate temperature whenever insulin sits out. If the exposure was brief and cool, it may still be fine within the product’s in-use window.
If you are unsure, review the product insert and consider whether performance has changed. When evaluating risk, compare the exposure to published storage limits. If you need a refresher on foundational steps, the Insulin Storage 101 article remains a helpful checklist for daily routines and labeling checkpoints (for a concise checklist, see Insulin Storage 101). For technique that supports consistent dosing, our guide on how to Use an Insulin Pen includes practical handling relevant to temperature consistency (for technique basics, see Use an Insulin Pen).
Recap
Safe handling hinges on temperature control, time tracking, and visual checks. Write start dates on opened containers, protect insulin from heat, and avoid freezing at all costs. When exposures happen, document details and compare against the label’s temperature and time limits. Replace suspect insulin rather than risking erratic glucose patterns.
Build routines that make errors less likely. Use insulated cases during commutes, store backups thoughtfully, and keep educational references handy. When planning travel, carry supplies on your person and prepare for screening. If you suspect damage or see unusual glucose responses, speak with your healthcare provider before adjusting doses or timing.
Tip: A small digital thermometer in your case makes temperature monitoring automatic and objective.
This content is for informational purposes only and is not a substitute for professional medical advice.