Understanding the link between magnesium and diabetes can help you make informed, practical choices. This guide reviews the evidence, compares supplement forms, and outlines cautious dosing ranges. It also covers safety, interactions, and how to discuss supplementation with your care team.
Key Takeaways
- Relationship overview: Magnesium and diabetes are connected through insulin action and glucose metabolism.
- Form matters: Glycinate and citrate are well tolerated; oxide is less bioavailable.
- Dose carefully: Stay within established limits and consider diet first.
- Check interactions: Diuretics and certain conditions can alter magnesium balance.
Magnesium and Diabetes: What the Evidence Says
Magnesium participates in hundreds of enzymatic reactions. In glucose metabolism, it helps insulin signaling and supports cellular glucose transport. Observational studies link lower magnesium intake to higher rates of type 2 diabetes. Supplement trials show small, inconsistent improvements in fasting glucose or insulin sensitivity, often in people with low baseline intake.
Large clinical guidelines urge caution with supplements. They emphasize lifestyle measures first and individualized care. For context on recommended intakes, forms, and safety thresholds, see the NIH ODS magnesium fact sheet (NIH ODS magnesium fact sheet). For general guidance on adjunctive therapies in diabetes, the ADA Standards of Care provide high-level recommendations (ADA Standards of Care).
How Magnesium Supports Glucose and Insulin Physiology
Magnesium stabilizes ATP (cellular energy), which insulin pathways use to move glucose into muscle and liver cells. It also modulates insulin receptor activity and downstream kinases. In plain language, adequate magnesium helps insulin work properly, supporting steadier blood sugar patterns. Mild deficiency may worsen insulin resistance, particularly when diet quality is low.
People often ask which magnesium is best for insulin resistance. Research suggests that any well-absorbed form can help replete levels, but overall dietary pattern and total intake matter more than the specific salt. For a structured food approach that complements supplements, see Best Diet for Insulin Resistance, which outlines meal patterns that reduce insulin load (Best Diet for Insulin Resistance).
Choosing a Magnesium Form: Glycinate, Citrate, Oxide, or Others
Not all magnesium salts act the same. Magnesium glycinate (chelated to glycine) is gentle on the stomach and commonly used for individuals sensitive to laxative effects. Magnesium citrate is well absorbed and slightly more likely to loosen stools. Magnesium oxide contains more elemental magnesium by weight but is less bioavailable and can cause gastrointestinal upset at higher doses.
Many people wonder, can diabetics take magnesium glycinate. In general, this form is considered well tolerated, but suitability still depends on kidney function, medications, and individualized targets. For a broader nutrition lens, our article on Plant-Based Nutrition discusses how whole foods support metabolic health, which may reduce reliance on supplements over time (Plant-Based Nutrition).
Dosing, Safety, and Interactions
Safe dosing depends on age, diet, kidney function, and co-medications. The Tolerable Upper Intake Level (UL) for supplemental magnesium is 350 mg/day for adults, not counting food sources. Intakes above this can cause diarrhea and cramping. People frequently ask how much magnesium should a diabetic take daily. A cautious approach is to prioritize food sources first, then consider low-to-moderate supplemental amounts within the UL, with clinician guidance.
Drug interactions can change magnesium balance. Loop and thiazide diuretics may increase magnesium losses; proton-pump inhibitors can reduce intestinal magnesium over time. For medication context, see Furosemide when reviewing loop diuretic effects and electrolyte monitoring strategies (Furosemide). Combination antihypertensives such as Ramipril HCTZ include a thiazide component, which may also affect levels; see that product page for class context (Ramipril HCTZ). For detailed safety and UL information, refer to the NIH ODS professional factsheet (NIH ODS magnesium fact sheet).
Who Might Benefit: Prediabetes, Type 1, Type 2, and PCOS
People with low dietary intake, prediabetes, or insulin resistance may benefit from repleting magnesium. Small trials suggest modest improvements in fasting glucose or HOMA‑IR when baseline intake is inadequate. Discussions about the best magnesium for type 2 diabetes should focus on correcting deficiency with a well-absorbed form, alongside diet quality, physical activity, and medication adherence.
Beyond type 2, insulin resistance is also common in polycystic ovary syndrome. While evidence for magnesium in PCOS is still emerging, improving overall micronutrient status may support metabolic markers. For food-forward strategies in prediabetes, see Low-Carb Veggies for Diabetes for examples of fiber-rich options that lower glycemic load (Low-Carb Veggies for Diabetes). For additional lifestyle guidance, the Legume Advantage article shows how pulses help with satiety and glucose control (Legume Advantage).
Practical Tips: Food Sources, Labs, and Monitoring
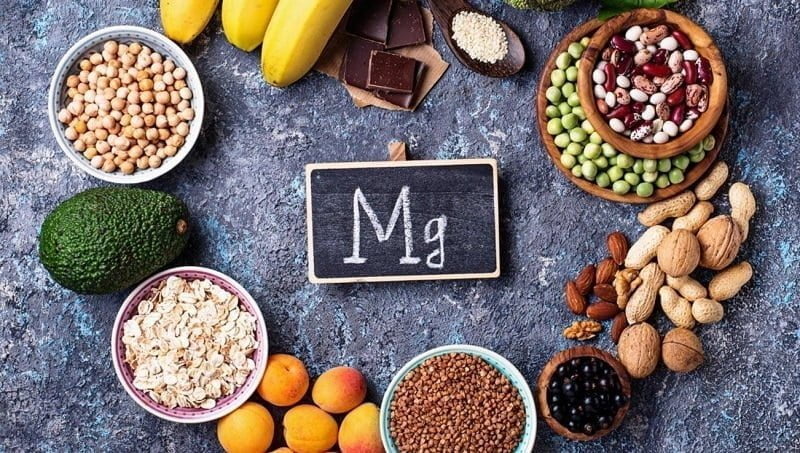
Food-first strategies reduce the need for high-dose supplements. Nuts, seeds, whole grains, legumes, and leafy greens provide consistent magnesium with fiber, potassium, and phytonutrients. Tofu and beans are reliable sources; for soy-based protein ideas, see Tofu for Diabetics: Nutrition and Benefits to build balanced meals that support glucose control (Tofu for Diabetics).
Standard serum magnesium can appear normal even when body stores are low. Clinicians may consider red blood cell magnesium or a trial of dietary repletion when suspicion is high. Some patients ask about magnesium for diabetic neuropathy. Evidence remains limited and mixed; maintaining overall nutritional adequacy and glucose stability remains the cornerstone. For supplement comparisons and storage tips across vitamins, browse our Vitamins Supplements category for broader context (Vitamins Supplements).
Medication Considerations
Magnesium and diabetes medication should be coordinated thoughtfully. Supplements may slightly affect absorption of certain drugs when taken together; spacing doses by two hours is a common practical approach. For example, people using GLP‑1 receptor agonists still rely on diet and micronutrients for comprehensive care. To understand how GLP‑1s fit into therapy, see Ozempic Semaglutide Pens for an overview of this class (Ozempic Semaglutide Pens) and Rybelsus Semaglutide Pills for oral options that may affect appetite and postprandial glucose (Rybelsus Semaglutide Pills).
Insulin users and those on incretin therapies should monitor glucose trends when adding supplements, especially if diet or activity also changes. For another nutrition-related adjunct, see Cinnamon and Diabetes, which reviews potential glycemic effects and safety considerations compared with mineral supplementation (Cinnamon and Diabetes). If a weekly injectable is part of your regimen, the Trulicity Pens overview offers additional therapy background to inform shared decision-making with your clinician (Trulicity Pens).
Recap
Magnesium influences insulin signaling and glucose handling, and correcting low intake may help some people improve metabolic markers. Choose a well-absorbed form, aim for food-first strategies, and keep supplemental doses conservative unless otherwise directed. Account for kidney function and possible drug interactions, especially with diuretics. Finally, align supplementation with diet, activity, and prescribed therapies for balanced, safe care.
Note: Positioning supplements as replacements for proven therapies can be risky. Treat them as adjuncts, and revisit the plan as labs, diet, and symptoms change.
This content is for informational purposes only and is not a substitute for professional medical advice.