Managing type 2 diabetes often requires stepwise, evidence-based choices. This guide explains what the medicine does, when to start it, how to dose it, and what to watch. You will also find comparisons, safety warnings, and combination options for long-term care planning.
Key Takeaways
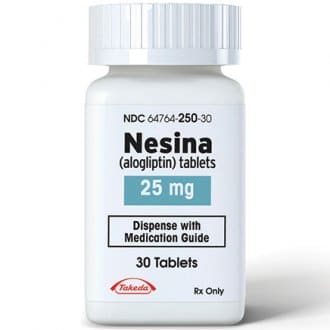
- Brand overview: nesina is a DPP-4 inhibitor used alongside diet and exercise.
- Renal function matters: dose reductions may be needed with reduced eGFR.
- Safety first: monitor for pancreatitis signs, liver injury, and heart failure.
- Combination therapy: pairs with metformin or TZDs when A1C targets are unmet.
- Switching options: compare class peers before changing to another agent.
What Is Nesina? Class, Action, and Indication
This medicine is a dipeptidyl peptidase-4 (DPP-4) inhibitor (enzyme blocker) approved for adults with type 2 diabetes. It enhances incretin hormones, which increase insulin release and reduce glucagon after meals. The net effect can help lower post-meal and fasting glucose without significant hypoglycemia when used alone.
Clinicians generally consider this class when metformin is not tolerated or as an add-on when A1C remains above goal. It is not for type 1 diabetes or diabetic ketoacidosis. It may be used with metformin, thiazolidinediones (TZDs), or insulin under careful supervision.
Who May Benefit and When to Use
Adults with type 2 diabetes who need additional A1C reduction and prefer an oral option may benefit. The class can suit patients who are leaner, are at hypoglycemia risk with sulfonylureas, or cannot tolerate gastrointestinal effects from metformin. Weight neutrality is common, which some patients prefer.
Clinicians assess cardiovascular status, kidney function, hepatic history, and pancreatitis risk before initiation. In patients with established cardiovascular disease, agents with proven cardiovascular benefit, such as SGLT2 inhibitors or GLP-1 receptor agonists, may be prioritized. The class remains a reasonable option when those therapies are not suitable or require augmentation.
Nesina Dosage and Titration Basics
Standard practice is to start with the labeled dose and adjust only for renal function. The label includes guidance for mild, moderate, and severe kidney impairment. To reduce dosing errors, clinicians align dosing with current estimated glomerular filtration rate (eGFR) trends and re-check periodically.
When discussing practical adjustments, clinicians often review concomitant medicines, hypoglycemia history, and A1C targets. A simple, consistent regimen supports adherence. If therapy is part of combination treatment, timing and pill burden should be streamlined. Always follow the approved FDA prescribing information for specific nesina dosage details and renal adjustments.
Kidney and Liver Considerations
Renal dosing adjustments are based on eGFR thresholds. Patients with moderate or severe renal impairment usually require a lower daily dose. Because kidney function can change with age, dehydration, or intercurrent illness, schedule periodic eGFR assessments and adjust dosing accordingly. If acute kidney injury occurs, reassess therapy and contributing medicines.
Hepatic impairment requires caution. If unexplained elevations in liver enzymes occur, evaluate for alternative causes and consider interruption. The class has rare postmarketing reports of hepatic injury. Baseline liver tests can guide monitoring, especially in patients with known hepatic disease or polypharmacy.
Comparisons and Switching
When comparing class peers, efficacy across DPP-4 inhibitors is generally similar for A1C lowering. Gastrointestinal tolerance is usually good, and weight effects are neutral. Differences often relate to renal dosing needs, pill strengths, and combination products available with metformin or TZDs.
Patients and clinicians sometimes weigh Nesina vs. Januvia Differences for formulation and dosing nuances, especially when switching within the class. For a broader look at class effects and expectations, see the DPP-4 Inhibitors Guide for symptom patterns and monitoring pointers. If options beyond DPP-4 inhibitors are considered, the Oral Diabetes Medications overview provides context on alternative pathways and add-on strategies.
Adverse Effects and Safety Warnings
Common reactions are usually mild, including nasopharyngitis and headaches. Hypoglycemia risk increases when combined with insulin or sulfonylureas, so consider dose adjustments of those agents. Rare but serious events have been reported across the class, such as pancreatitis, severe joint pain, and bullous pemphigoid.
Clinicians counsel on pancreatitis symptoms (persistent, severe abdominal pain) and heart failure signs (shortness of breath, swelling). The medicine carries class warnings reflected in the FDA prescribing information, which includes cautions for hospitalization for heart failure in susceptible patients. For practical symptom tracking and adverse event planning, align monitoring with the ADA Standards of Care that outline routine safety checks for glucose-lowering drugs.
As part of counseling, explain that alogliptin side effects can occur, though most users tolerate treatment. Encourage prompt reporting of rash, blistering, jaundice, dark urine, or new edema. If severe events arise, stop the drug and evaluate other causes while providing appropriate care.
Interactions and Combination Therapy
This agent is commonly paired with metformin for complementary mechanisms. Fixed-dose combinations simplify regimens and may help adherence. For background on the alogliptin–metformin pairing, see the Kazano Overview, which explains when a dual agent makes practical sense. If metformin alone is insufficient, adding a DPP-4 inhibitor can reduce pill count compared with separate tablets.
Thiazolidinediones are another pairing option, available in certain markets as a fixed-dose with pioglitazone. The brand oseni is an example of that combination. When choosing among combination tablets, compare dose strengths and renal considerations; for dose-strength context and formulations, review Kazano 12 5 1000mg 56 Tablets and extended-release metformin options such as Glumetza. If a patient needs metformin with sitagliptin instead, once-daily Janumet XR provides a relevant counterexample for regimen simplicity.
Costs, Brands, and Generics
Brand and generic availability varies by region and payer. Formularies may favor certain agents based on negotiated coverage rather than clinical differences. Patients should work with clinicians and payers to identify the covered option with the simplest dosing and acceptable copay.
When discussing brand and generic names, confirm the active ingredient on the label and the manufacturer. For quick product context and pack sizes, see Nesina 28 Tablets along with our broader Diabetes Medications List for class alternatives. If budgeting is an issue, pharmacists can clarify therapeutic equivalents and formulary tiers. Talk with your clinician or plan about nesina generic availability and any prior authorization steps.
Practical Monitoring and Dose Limits
Before and after initiation, check A1C every 3 months until stable, then at least twice yearly. Monitor fasting glucose, weight, and symptoms that suggest side effects. Review concomitant therapies that may raise hypoglycemia risk. Assess eGFR at baseline, then periodically, and after any intercurrent illness affecting kidney function.
To avoid overdosing, confirm strength, frequency, and renal status at each visit. Document any interruptions during acute illness, then re-titrate safely. Educate patients on sick-day rules, dehydration risks, and when to hold certain drugs. Dose limits are defined by the product label; clinicians should be aware of the alogliptin maximum dose and avoid exceeding it during switches or when combining treatments.
Patient Education and Adherence Supports
Clear counseling improves adherence and reduces safety risks. Align the dose with daily routines such as breakfast, and use pill organizers or reminder apps if needed. Reinforce diet and activity goals, since pharmacotherapy works best alongside lifestyle measures. Explain expected benefits and realistic timelines for A1C change.
Offer written instructions in plain language and confirm understanding with teach-back. Share practical reading that supports long-term planning, such as the Benefits of Nesina article for mechanism and outcomes. For broader condition context, the Type 2 Diabetes category collects related guidance across diet, monitoring, and medicines. When considering alternative add-on classes, review SGLT2 options like Dapagliflozin and combination formulations such as Invokamet for comparative pathways.
Recap
This DPP-4 inhibitor can lower glucose modestly, with a neutral weight profile and a generally low hypoglycemia risk when used alone. Its role is strongest as an add-on for patients who need incremental A1C improvement while preserving simplicity and tolerability.
Choose patients carefully, adjust for kidney function, and monitor for rare but serious adverse effects. Compare within and beyond the class to match individual goals, coverage, and comorbidities. When used thoughtfully, it can be a steady component of multi-year diabetes care.
Note: Always verify renal function and current medications before starting or adjusting therapy. Reassess after any acute illness or hospitalization.
This content is for informational purposes only and is not a substitute for professional medical advice.