Choosing carbohydrates wisely can stabilize post-meal glucose and support long-term health. This guide explains fiber-rich options, portion targets, simple meal ideas, and label reading. We use current nutrition guidance to help you translate theory into everyday choices. Early on, we define what are good carbs for diabetics and how to use them within a balanced plate.
Key Takeaways
- Favor fiber-dense carbs: vegetables, legumes, intact grains, and berries.
- Spread carbs through the day; match intake with activity and meds.
- Read labels for serving size, total carbs, and fiber grams.
- Build meals with protein, healthy fats, and non-starchy vegetables.
- Use practical tools to plan portions and monitor glucose responses.
What Are Good Carbs for Diabetics
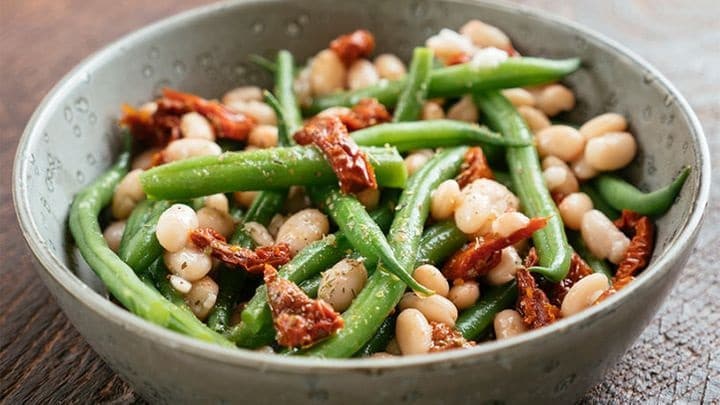
In clinical nutrition, carbohydrates vary by structure and fiber content. Slowly digested options with higher fiber (dietary fiber) and intact cell walls usually produce a steadier glucose curve. Think beans, lentils, chickpeas, steel-cut oats, barley, quinoa, and non-starchy vegetables like broccoli and leafy greens. Lower-sugar fruits such as berries, apples, and pears also fit well in moderate portions.
These choices provide vitamins, minerals, and resistant starch, which may improve insulin sensitivity. Pairing carbs with protein and unsaturated fats further blunts spikes by slowing gastric emptying. For broader nutrition context across conditions, our Diabetes Articles category offers structured guides for different eating patterns; see Diabetes Articles for topic overviews and deeper reading.
Complex Carbs and Glycemic Impact
Complex carbohydrates are formed from longer chains of sugars, often packaged with fiber and phytonutrients. Whole-food sources generally digest more slowly than refined grains, which can support steadier postprandial (after-meal) readings. Building meals around legumes, intact whole grains, and vegetables may also improve satiety, which helps with weight management.
Because examples help with planning, a complex carbs list can guide grocery choices and meal prep. Compare steel-cut oats to instant packets, or intact barley to quick-cook couscous. For plant-forward eaters, our Vegan Diet and Diabetes article offers practical swaps and menu ideas to keep fiber high while meeting protein needs.
For high-level background on carbohydrate quality and blood glucose, the CDC provides balanced guidance on carbohydrates and diabetes management; see the CDC’s overview for foundational principles (CDC carbohydrate guidance).
Portion Planning and Carb Targets
Carb needs are individual and depend on age, activity, body size, medications, and glycemic goals. Many adults spread intake across three meals and one or two snacks, pairing carbs with protein and vegetables. Dietitians often start by assessing current patterns, then adjust total carbohydrates while monitoring glucose trends. Using a plate method—half non-starchy vegetables, one-quarter protein, one-quarter whole grains or starchy vegetables—keeps portions consistent.
When discussing numeric goals, ask your clinician for personalized ranges. If you track daily totals, consider how many carbs per day for diabetic aligns with your treatment plan and exercise schedule. For people targeting weight control, see Lose Weight With Diabetes for behavioral strategies alongside nutrition planning that avoids under-fueling during the week.
For practical, clinician-reviewed targets and examples, the ADA outlines carbohydrate counting and meal planning fundamentals; review the ADA’s meal planning basics for context (ADA carb overview).
Good Carbs vs. Bad Carbs
The terms “good” and “bad” are oversimplified, but the concept helps with triage. Prioritize carbs that bring fiber, water, and micronutrients—vegetables, legumes, and intact grains. Limit refined grains and concentrated sugars, especially when they crowd out nutrient-dense foods. Many people do well by swapping white bread for whole-grain sourdough or choosing brown rice or quinoa instead of white rice.
Fructose-heavy beverages, pastries, and candy offer energy but little nutritional value. A practical frame is frequency and portion: occasional treats, small amounts, and pairing with a protein can reduce glycemic impact. For insulin resistance–focused guidance that links quality carbs with metabolic health, see Best Diet for Insulin Resistance to align food choices with cardiometabolic goals. This section includes the comparison idea captured by good carbs vs bad carbs but encourages nuance.
Breakfast and Practical Meal Ideas
Morning meals set the tone for your day’s glucose curve. Combine slow-digesting carbs, protein, and healthy fats. Examples include steel-cut oats with chia and walnuts, Greek yogurt with berries and flaxseed, or a vegetable omelet with a slice of whole-grain sourdough. On busier days, a whole-grain wrap with eggs and spinach travels well.
To keep the first meal consistent, plan a simple breakfast for diabetics using 20–40 grams of carbohydrate, depending on your needs and clinician advice. If you include dairy at breakfast, review Diabetes-Friendly Dairy for calcium sources and tips on lactose content. When considering sweetened beverages, Chocolate Milk and Diabetes explains how sugars, protein, and timing may affect post-meal readings, offering balanced guidance for occasional use.
Sample Plates to Mix and Match
Use a mix-and-match approach when planning. For example, pair half a plate of non-starchy vegetables with one-quarter protein and one-quarter whole grain. Rotate proteins—eggs, tofu, fish, or lean poultry—and swap grains like quinoa, farro, or barley. For fruit, choose berries or an apple, then add nuts or seeds for texture. This structure keeps variety high while stabilizing energy mid-morning, which supports activity or work demands without large glucose swings.
Foods and Patterns to Limit
Strong evidence links sugar-sweetened drinks, refined grains, and ultra-processed foods with higher glycemic excursions. Desserts, pastries, and white breads can be enjoyed sparingly, but frequent use may displace fiber-rich options that protect cardiometabolic health. Consider timing as well: having sweets with a meal rather than alone lessens spikes.
When choosing fruit, portion size matters as much as type. For examples of items that may spike glucose, see Fruits for Diabetics To Avoid for practical fruit selection and sizing tips. For broader pantry choices and cooking patterns, review what foods to avoid with diabetes within your household’s routines and budget. This section helps you swap smarter rather than eliminate entire food groups.
Carb Counting, Labels, and Tools
Label reading starts with serving size, total carbohydrate, and dietary fiber. Subtracting fiber from total carbohydrates provides net carbs, a practical estimate of digestible carbohydrate. Track patterns with a food log and use glucose data to identify meals that fit your targets. Apps can be helpful, but simple notes and a glucose meter or continuous monitor work well.
If you prefer printable tools, a diabetes carb counting chart pdf can reinforce label reading and portion decisions. When you use sweeteners, our Healthiest Sweetener Tips summarizes options and how each may affect taste and calorie intake. For lipid awareness alongside carbohydrate choices, Triglycerides and Diabetes explains how diet patterns can influence blood lipids over time, which matters for cardiovascular risk reduction.
The National Institute of Diabetes and Digestive and Kidney Diseases offers a practical overview of carbohydrate counting with examples; see their educational resource for step-by-step guidance (NIDDK carb counting).
Special Cases: Exercise, Growth, and Hypoglycemia
Activity, growth periods, illness, and medication changes alter carbohydrate needs. Endurance exercise often increases carb requirements before, during, or after sessions, while lighter movement may not. Monitor with your clinician when adjusting carb timing around sports or long work shifts. Keep rapid-acting carbohydrate sources available if you use insulin or medications that can induce hypoglycemia.
Many care teams teach the “15–15” approach to mild lows: 15 grams of fast carbohydrate, then recheck in 15 minutes. The idea that 15g of carbohydrates will raise blood sugar by a predictable amount is a guideline, not a guarantee; responses vary by person and context. For people using GLP-1 therapies, the Ozempic Diet Plan and the Mounjaro Diet Guide explain how to align meal composition with appetite changes and glycemic goals, helping you tailor carb timing around medication effects.
For additional nutrition and lifestyle frameworks, our Living With Diabetes Tips article offers daily routines and planning prompts that you can adapt across workdays and weekends without rigid rules.
Recap
Carbohydrates belong in a balanced diabetes eating plan. The most helpful change is shifting your carb pattern toward higher-fiber, minimally processed foods while keeping portions consistent. Pair carbs with protein and healthy fats, and adjust timing around activity or medication effects. Use labels and simple planning tools to track patterns, then refine based on your glucose data.
Meal-by-meal consistency adds up over weeks. You can rotate choices to keep meals satisfying while staying within your targets. When you need deeper dives on fruit, dairy, or sweeteners, explore our linked guides for practical examples and next steps. If you have complex needs or new medications, ask your care team for personalized direction before making major changes.
Note: Nutrition needs vary. Discuss significant diet changes with your healthcare professional, especially if you take glucose-lowering medications.
This content is for informational purposes only and is not a substitute for professional medical advice.