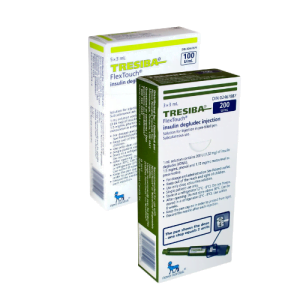
Intermediate-acting insulins are a critical component in the management of diabetes, providing a balance between rapid-acting and long-acting insulins. These insulins help maintain baseline insulin levels and manage blood glucose levels throughout the day. Understanding their pharmacological profile is essential for both patients and healthcare providers.
Types of Intermediate-Acting Insulin
The most common types of intermediate-acting insulin include:
- NPH (Neutral Protamine Hagedorn) Insulin: This is the most widely used intermediate-acting insulin. It is often combined with short-acting insulin to provide better glucose control.
Pharmacological Profile
1. Onset of Action
Intermediate-acting insulins typically start to work within 1 to 3 hours after injection.
2. Time to Peak Effect
The peak glucose-reducing effect occurs between 4 to 8 hours after administration.
3. Total Duration of Action
The effects of intermediate-acting insulin can last between 14 to 24 hours, making it suitable for maintaining baseline insulin levels.
Additional Pharmacological Details
- Distribution: Intermediate-acting insulin is distributed rapidly in the extracellular fluid.
- Metabolism: It is primarily metabolized in the liver, with some metabolism occurring in the kidneys and muscles.
- Excretion: The metabolites of intermediate-acting insulin are excreted in the urine.
Clinical Considerations
When using intermediate-acting insulin, it is essential to consider the timing of doses in relation to meals and daily activities to optimize blood glucose control. Patients should work closely with their healthcare providers to adjust dosages and schedules based on their individual needs and responses to insulin therapy.
Intermediate-acting insulin plays a vital role in diabetes management, offering a balance that helps to maintain steady insulin levels and prevent both hyperglycemia and hypoglycemia. Proper understanding and utilization of these insulins can significantly improve the quality of life for individuals with diabetes.
Disclaimer: Please note that the contents of this community article are strictly for informational purposes and should not be considered as medical advice. This article, and other community articles, are not written or reviewed for medical validity by Canadian Insulin or its staff. All views and opinions expressed by the contributing authors are not endorsed by Canadian Insulin. Always consult a medical professional for medical advice, diagnosis, and treatment.