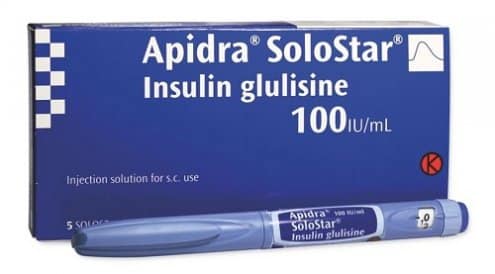
The Apidra SoloStar Pen delivers insulin glulisine, a rapid-acting mealtime insulin. Understanding apidra insulin side effects helps you recognize problems early and use this therapy more safely. This guide reviews common reactions, serious warning signs, and practical steps for safer day-to-day use.
For a deeper look at indications and timing, see Apidra SoloStar Pen Uses for context on when it fits into care. You can also review Rapid-Acting Insulin Solution for pharmacology basics that influence side-effect patterns.
Key Takeaways
- Common reactions: mild site redness, headache, or edema.
- Serious risks: severe hypoglycemia, allergic reactions, low potassium.
- Interaction watch: alcohol, steroids, and beta blockers.
- Practical safety: rotate sites, carry carbs, check labels.
- Storage matters: avoid heat and freezing; follow expiry.
What Apidra SoloStar Is and How It Acts
Apidra (insulin glulisine) is a rapid-acting insulin for mealtime glucose spikes. It starts working quickly and is usually taken within 15 minutes before or soon after eating. You may hear clinicians discuss onset and peak to guide timing. For details on absorption and kinetics, review the manufacturer’s prescribing information, which outlines clinical pharmacology and safety.
Clinically, Apidra onset and peak inform dose timing and low blood sugar prevention. Typical onset is minutes, with a peak effect about one to two hours later, and a shorter overall duration than basal insulin. These timepoints matter when coordinating meals, activity, and correction doses. For a broader overview of fast insulins in daily life, see Understanding Apidra Insulin to connect action profiles with day-to-day symptoms.
Understanding apidra insulin side effects
Side effects range from mild and temporary to serious and urgent. Common issues include injection site redness, small bruises, and transient headaches. Some users notice edema (fluid retention), especially when glycemic control improves quickly. These effects usually ease with time, site rotation, and consistent technique.
Serious adverse effects are less common but need prompt attention. These include severe hypoglycemia (low blood sugar), significant allergic reactions, and hypokalemia (low potassium). Severe, persistent, or atypical symptoms should prompt urgent evaluation. When in doubt, review the basic signs and compare with your typical response patterns. A practical primer on meal timing strategies is covered in Mealtime Flexibility, which can reduce variability that drives side effects.
Hypoglycemia, Low Potassium, and Weight Changes
Low blood sugar can occur with any rapid insulin. Apidra hypoglycemia risk rises with meal mismatches, unexpected activity, alcohol, dosing errors, or impaired kidney function. Typical early symptoms include shakiness, sweating, and fast heartbeat. Severe episodes may lead to confusion or loss of consciousness. Keep fast carbohydrates available and consider carrying glucagon as advised by your care team.
Hypokalemia (low potassium) may appear with aggressive insulin dosing, especially if you have other potassium-shifting risks. Signs can include muscle weakness or palpitations. Edema and modest weight gain may occur as glycemic control improves, due to osmotic shifts and fluid retention. For driving and safety-sensitive tasks, the ADA Standards of Care provide guidance on preventing lows while operating vehicles or equipment.
Injection Site and Allergic Reactions
Local skin issues are among the most frequent complaints. Apidra injection site reactions include redness, stinging, or mild swelling. Rotate sites within the same body area to reduce irritation, and avoid injecting into scarred or lipodystrophic (fat-redistribution) tissue. Proper needle length and gentle technique help minimize trauma.
Allergic reaction symptoms can include widespread hives, facial swelling, wheezing, or severe dizziness. Anaphylaxis (a severe allergic reaction) is rare but life-threatening and requires emergency care. If local reactions persist or worsen, discuss alternative sites, delivery methods, or formulations. For a broader insulin comparison that may inform tolerability, see Not All Insulin Products Are Created Equal to understand differences across classes.
Interactions, Alcohol, and Contraindications
Medication combinations can alter insulin needs. Apidra drug interactions may involve steroids, some antipsychotics, and decongestants, which can raise glucose. Conversely, certain antibiotics, ACE inhibitors, and salicylates can enhance insulin’s effect, increasing low-blood-sugar risk. Beta blockers may blunt adrenergic warning signs, delaying recognition of a drop. Review all prescriptions and supplements with your clinician and pharmacist.
Alcohol can unpredictably change glucose levels, especially with missed meals or intense exercise. People with known hypersensitivity to insulin glulisine or any excipient should not use this product. Active, untreated hypoglycemia is also a contraindication. For detailed labeling on interactions and contraindications, consult the official prescribing information. If you are evaluating alternatives, Apidra Alternatives can help frame discussion points with your care team.
Special Populations and Activities
Pregnancy and breastfeeding require individualized plans. Available data suggest rapid-acting analogs can be used with close monitoring, but risk-benefit decisions remain personalized. Discuss glucose targets, nocturnal lows, and any changes to correction factors. During breastfeeding, watch for increased sensitivity and adjust meal timing as needed to reduce symptomatic lows.
Older adults, people with renal or hepatic impairment, and those in safety-sensitive jobs may need extra precautions. Before driving or operating machinery, confirm stable glucose and intact awareness of hypoglycemia. For sport or heavy labor, consider pre-activity checks, carbohydrate planning, and post-activity monitoring. Category reviews like Type 1 Diabetes and Type 2 Diabetes provide broader context for managing risks across different populations.
Dosing Errors, Missed Doses, and Overdose
Mealtime insulins require careful label checks to avoid mix-ups with basal doses. If a dose is missed and the meal has passed, Apidra missed dose what to do generally depends on glucose level, time since eating, and clinician advice. Avoid stacking multiple correction doses close together. Use meters or CGMs to guide next steps and reduce rebound swings.
Overdose symptoms can include rapid-onset hypoglycemia, confusion, or loss of consciousness. If severe, emergency treatment may include glucagon and medical evaluation. Consider keeping an action plan visible and sharing it with family members. For an overview of insulin classes to prevent product confusion, see Navigating the Insulin Landscape for terminology and device differences that reduce errors.
Practical Error-Prevention Tips
Separate mealtime and basal pens physically to prevent selection errors. Confirm the pen label, dose window, and units before each injection. Prep carbohydrates in advance when eating out to handle unexpected delays. Use reminders or smartphone logs to mark injection time and site. When starting a new pen, prime per device instructions to ensure dose accuracy. Device-specific details for this product are summarized under Apidra SoloStar Pens, which can help you match technique with manufacturer guidance.
Storage, Handling, and Pump Considerations
Proper temperature control preserves potency and limits variability. Apidra storage and handling includes keeping unopened pens refrigerated and avoiding freezing or direct heat. In-use pens are typically stored at room temperature within labeled time limits. Protect from sunlight and recap needles immediately after dosing to reduce contamination and leakage.
Pump users should monitor for site occlusions, unexpected highs, and skin irritation around infusion sets. If insulin has been exposed to heat, replace the cartridge or pen and reassess glucose. For specific thresholds and duration limits, see Insulin Storage 101, which clarifies temperatures and discard times. Technique refreshers are also available in Understanding Apidra Insulin to align handling with expected performance.
Comparing Tolerability With Other Rapid-Acting Insulins
Rapid analogs share many class effects, though individual response varies. Some people tolerate one product better than another due to formulation or absorption differences. Reviewing similarities and differences can guide conversations about alternatives if side effects persist despite good technique. For a structured comparison, see Apidra vs Humalog for balanced pros and cons.
Considering device preferences can also influence choice and adherence. If your clinician suggests a switch, reviewing devices such as Humalog KwikPen or formulations like Novorapid Vials can clarify what may change in practice. For meal timing strategies that support tolerability across brands, revisit Mealtime Flexibility to align dose timing with eating patterns.
Recap
Most side effects are mild and manageable with consistent technique and monitoring. Stay alert for severe lows, allergic symptoms, and persistent site issues. Use labeling, timing, and storage practices to reduce avoidable problems. When patterns change, review medications, activity, and alcohol, then discuss adjustments with your care team.
Note: For complex scenarios or recurring reactions, document dose timing, meals, and activity to identify triggers.
This content is for informational purposes only and is not a substitute for professional medical advice.