Choosing the best GLP-1 for weight loss in 2025 requires balancing efficacy, tolerability, and access. These medications target appetite and gastric emptying to help reduce caloric intake. New oral candidates widen the field, while weekly injectables remain core options. This guide summarizes mechanisms, dosing fundamentals, safety signals, and how to decide next steps.
Key Takeaways
- Mechanism first: appetite control and delayed gastric emptying drive results.
- Pick by goals: weight, metabolic profile, and comorbidities matter.
- Safety counts: gastrointestinal effects and rare risks require monitoring.
- Access and fit: dosing schedule and formulation drive adherence.
What GLP-1 Agonists Do and Why They Matter
Glucagon-like peptide-1 receptor agonists lower appetite, slow gastric emptying, and support lower energy intake. In clinical and real‑world settings, they can reduce body weight when combined with nutrition and activity changes. People often report earlier fullness and fewer cravings, which helps with consistency.
Used as glp-1 for weight loss, these agents also influence metabolic health. Many show improvements in glycemic control and cardiometabolic markers. For broader lifestyle context that complements medication, see Weight Management for structured, sustainable strategies.
Determining the best GLP-1 for weight loss: Criteria and Context
No single option fits everyone. Selection hinges on measurable goals, concomitant conditions, and side‑effect tolerance. Weekly injectables suit people who prefer less frequent dosing and steady exposure. Oral candidates appeal to those avoiding injections, though food timing and adherence may be more sensitive.
Consider cardiometabolic profile, gastrointestinal tolerance, and access constraints. Comparative performance varies by molecule, dose, and adherence patterns. Pipeline orals could shift choices over time. For a head‑to‑head view of two oral strategies, see Orforglipron vs Rybelsus for practical distinctions on administration and effectiveness.
Comparing Injectable and Oral Options in 2025
Injectable products remain the dominant class due to consistent exposure and robust dosage ranges. Weekly dosing can simplify routines and reduce missed doses. Oral agents are evolving, offering needle‑free administration that some people prefer. Food timing and absorption can influence results, so counseling and reminders matter.
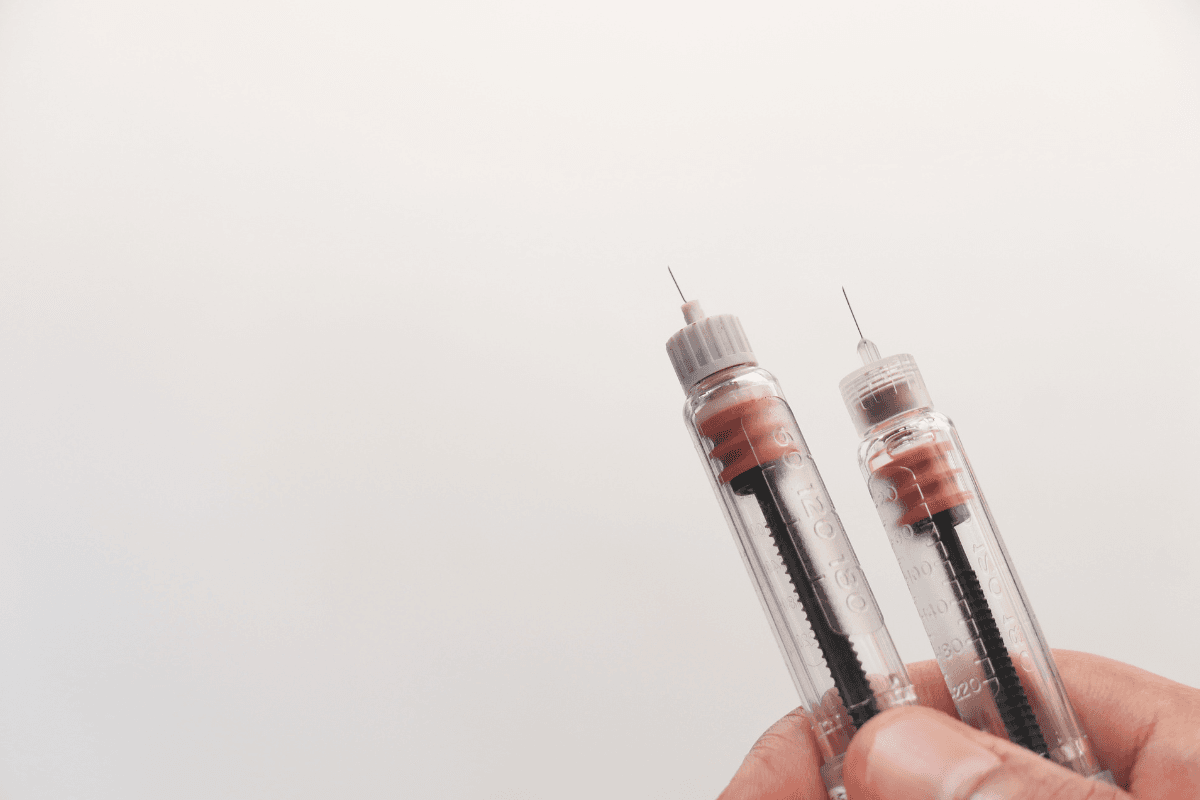
When reviewing a glp-1 drugs list, evaluate delivery route, titration flexibility, and known tolerability. Weekly semaglutide and dual‑incretin options remain central choices. For weekly semaglutide specifics, see Wegovy for dose forms and indication details. For diabetes‑labeled semaglutide used in metabolic care, see Ozempic Semaglutide Pens for device and pen formats. If considering dual incretin therapy, review Mounjaro KwikPen for administration specifics and practical handling notes.
Dosing Basics and Safety Considerations
Dosing starts low and increases gradually to improve tolerability. Most programs escalate every several weeks, allowing the gut to adapt. People benefit from a structured plan that anticipates nausea, fullness, or reflux. A written schedule and food strategies can reduce setbacks and missed doses.
If you seek a visual overview, a semaglutide weight loss dosage chart can clarify titration steps and maintenance targets. However, product labels govern dosing and warnings. For official directions, review the FDA-approved labeling for Wegovy before starting or changing therapy. For dual‑incretin specifics and warnings, see the FDA label for Zepbound for formal guidance and contraindications.
Titration Across Brands
Different products escalate at different rates, and some have broader top doses. A slower titration may help people sensitive to gastrointestinal effects. Conversely, advancing too quickly can increase nausea, fullness, or vomiting. Using a standardized schedule, meal adjustments, and hydration often improves tolerance. Discuss new or persistent symptoms before moving up a dose. For duration planning and maintenance strategies, see How Long to Take Ozempic for a balanced overview of therapy timelines.
Side Effects and Risk Signals
Most glp-1 side effects involve the gastrointestinal tract. Nausea, early satiety, reflux, and constipation are common during dose escalation. Slow eating, smaller portions, and lower dietary fat can help. If symptoms persist or worsen, clinicians often pause or delay dose increases.
Rare risks include gallbladder events and pancreatitis, with thyroid C‑cell tumor warnings on labels. People with relevant histories should review contraindications and precautions before use. For practical management of a frequent symptom, see Wegovy and Constipation for supportive strategies and red‑flag guidance.
Special Populations and Non-Diabetic Use
Many candidates pursue weight control outside a diabetes diagnosis. Indications may include chronic weight management in adults with obesity or overweight plus risk factors. Clinicians assess BMI, comorbidities, and medication history before prescribing. They also confirm that lifestyle changes are feasible and supported.
Pregnancy, planned conception, and certain gastrointestinal or endocrine conditions require careful review. Some therapies carry specific warnings or contraindications tied to these situations. People with complex histories may need alternative approaches or slower titration. Ongoing monitoring helps confirm that benefits outweigh risks over time.
Pills and Supplements: What’s Realistic
There is one prescription oral option using the same active molecule as injectable semaglutide. It is taken daily with strict timing and fasting instructions. For formulation details and administration requirements, see Rybelsus Semaglutide Pills for a concise overview of tablet strengths.
Marketing claims around glp-1 pills and over‑the‑counter products can be confusing. Dietary supplements do not replicate receptor‑level effects or labeled outcomes. Some may assist general nutrition, appetite patterns, or energy, but evidence varies widely. Evaluate ingredients, evidence quality, and potential interactions before use.
Alternative Pharmacotherapy and OTC Aids
Non–GLP‑1 medications may help selected people who cannot tolerate incretin therapy. Options include agents that reduce absorption, modulate appetite, or affect reward pathways. Benefits, risks, and side‑effect profiles differ across classes. Discuss history of GI issues, hypertension, and mood disorders before choosing alternatives.
For an example of a combination therapy with central action, see Contrave Tablets for ingredient and dosing context. Insurance coverage and local availability will shape access. Over‑the‑counter products vary in evidence, so expectations should remain modest. Documenting side effects and weight trends helps determine whether to continue or change strategy.
How to Choose and Monitor Progress
Define goals first, then match the medication profile to needs. Consider expected weight change, glucose benefits, schedule fit, and side‑effect tolerance. Plan for dose ramps, food adjustments, and follow‑up intervals. Early course corrections help maintain momentum and reduce discontinuations.
Track weight, circumference, and symptom patterns every few weeks. If a plateau or regain appears after changes, evaluate adherence, dose timing, and nutrition first. For structured planning after dose adjustments or interruptions, see Ozempic Rebound for practical guardrails on maintenance.
Recap
GLP‑1–based therapies remain a cornerstone for evidence‑based weight management. Injectable and oral options serve different adherence preferences, while dosing plans and safety checks determine day‑to‑day success. Most people do best with gradual titration, proactive symptom management, and simple nutrition routines.
Choose an agent by goals, tolerability, and access, then review progress at set intervals. Use product labels for safety guidance and dosing boundaries. Keep expectations realistic, and document both benefits and side effects. With consistent monitoring, the approach can stay safe, sustainable, and aligned with priorities.
This content is for informational purposes only and is not a substitute for professional medical advice.