Please note: a valid prescription is required for all prescription medication.
Apidra Vials Product Overview and Safety
Start 2026 with savings: Use code SAVE10 for 10% OFF all RX meds. Jan–1 Mar. Ozempic from Canada and Mounjaro Vial not included. Offer valid until March 1st. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
Maximize your savings with Canadian Insulin: Buy 2 for a 10% discount, or stock up with 3 or more to unlock an incredible 20% off on your insulin needs.
$61.99
You save


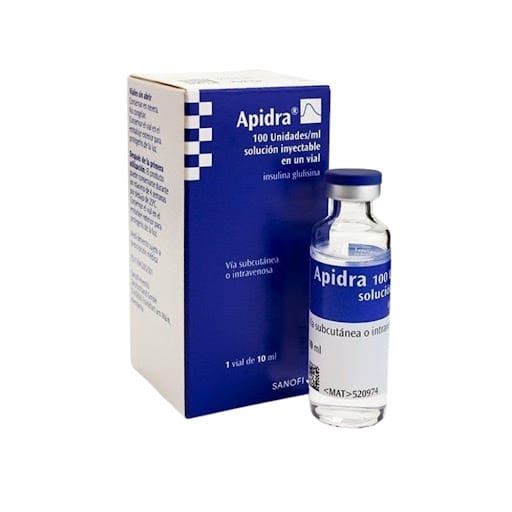
Apidra Vials are multidose vials of rapid-acting insulin glulisine used to help manage blood glucose around meals. They are typically used as part of a broader diabetes plan that can include basal insulin, nutrition planning, and monitoring. Some patients explore Ships from Canada to US pathways when they are reviewing access logistics, and this page summarizes label-aligned use, storage, and safety basics.
What Apidra Vials Is and How It Works
Insulin glulisine is a rapid-acting insulin analog (a lab-made form of insulin) designed to work quickly after injection. It helps lower blood glucose by supporting glucose entry into muscle and fat cells and by reducing glucose output from the liver. CanadianInsulin.com provides prescription referral support; licensed third-party pharmacies dispense where permitted.
This medicine is mainly used to cover the rise in blood glucose that occurs with meals. It is commonly paired with a longer-acting insulin to provide day-long baseline coverage. Insulin needs can shift with diet, activity, illness, stress, or changes in kidney or liver function. Because insulin has a narrow safety margin, changes in insulin type, device, or routine are usually done with clinician guidance and careful monitoring.
Why it matters: Rapid-acting insulins require planning around meals to reduce hypoglycemia risk.
Who It’s For
Insulin glulisine may be prescribed for people with type 1 diabetes and for some people with type 2 diabetes who need mealtime insulin. For background on these conditions, you can browse the Type 1 Diabetes Hub, the Type 2 Diabetes Hub, or the broader Diabetes Condition Hub. Age indications and specific labeling can vary by country, so the prescribing clinician will match the product to the patient’s situation.
This insulin is not appropriate for treating low blood sugar at the moment it is happening. It is also generally avoided in anyone with a known serious allergy to insulin glulisine or another ingredient in the formulation. If severe hypoglycemia occurs repeatedly or unpredictably, clinicians may reassess meal timing, injection technique, monitoring, and the overall regimen.
- Mealtime glucose control: used around eating
- Basal-bolus plans: often combined with long-acting insulin
- Not for acute lows: treat hypoglycemia with fast carbohydrates
- Allergy history: discuss prior reactions to insulin
Dosage and Usage
For Apidra Vials, dosing is individualized and based on factors such as meals, activity, and glucose targets set by a clinician. Rapid-acting insulin is often taken shortly before eating, and some labeling allows dosing soon after starting a meal in specific situations. The prescriber may also provide a correction approach for unexpected hyperglycemia, along with instructions for monitoring and follow-up.
Vials are used with U-100 insulin syringes, and the dose is measured in insulin units. Always confirm the syringe matches the concentration (U-100) to avoid a major dosing error. Injection is given subcutaneously (under the skin) in areas such as the abdomen, thigh, or upper arm, with routine site rotation to reduce lipodystrophy (lumpy or thickened skin). Do not share syringes, needles, or devices, even within a household.
Quick tip: Keep a consistent routine for handwashing, labeling, and dose double-checks.
Some people use rapid-acting insulin in an insulin pump. If a pump is part of care, follow the pump instructions for reservoir filling, infusion set changes, and troubleshooting. Any switch in insulin type or concentration should be reviewed with the clinician managing pump settings.
Strengths and Forms
Apidra Vials contain insulin glulisine as a clear, rapid-acting injectable solution. The most common presentation is U-100 insulin (100 units/mL) supplied as a multidose vial. Other presentations of insulin glulisine may exist (such as prefilled pens), and availability can differ by market and pharmacy.
Packaging identifiers like an NDC (National Drug Code) or DIN can vary by country and distributor. For the most accurate identifier, confirm the code printed on the carton and vial label, and keep that information with your medication list for clinic visits.
| Presentation | Concentration | How it’s used | Notes |
|---|---|---|---|
| Multidose vial | U-100 (100 units/mL) | Syringe dosing; sometimes pump reservoir filling | Follow label for in-use time limits |
| Prefilled pen | U-100 (100 units/mL) | Pen needles and dialed dosing | Separate product presentation; availability varies |
Storage and Travel Basics
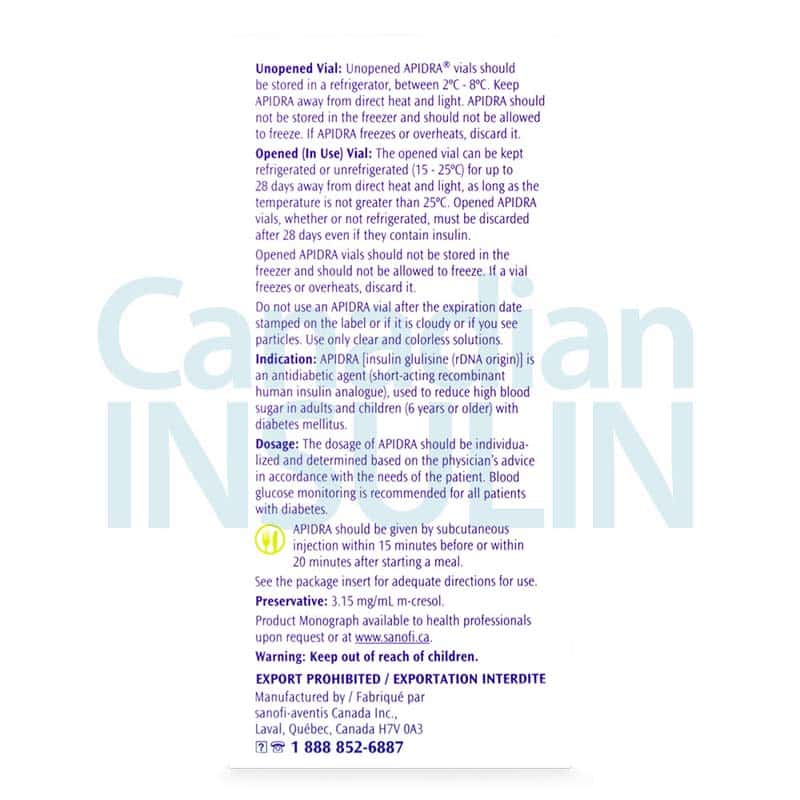
Proper storage helps insulin maintain its expected activity. Unopened insulin is commonly kept refrigerated and protected from freezing and direct light. Once in use, many insulins can be kept at controlled room temperature for a limited time, but the exact duration depends on the specific product instructions and the local labeling.
For Apidra Vials, check the package insert for the in-use expiration window and discard timing after first puncture. Avoid storing insulin in a very hot car, near heaters, or in direct sunlight. Before each dose, inspect the solution; rapid-acting insulin glulisine is typically clear and should not look cloudy or contain visible particles.
- Refrigerate unopened: avoid freezing temperatures
- Protect from heat: keep away from sunlight
- Inspect before use: confirm solution stays clear
- Plan for travel: pack temperature protection
When traveling, carry insulin and supplies in your hand luggage when possible, along with a copy of the prescription and a simple medication list. If you use a continuous glucose monitor or pump, bring backup supplies in case of device issues.
Side Effects and Safety
The most common safety concern with any insulin is hypoglycemia (low blood sugar). Symptoms can include shakiness, sweating, hunger, headache, confusion, blurred vision, or irritability. Apidra Vials can also cause injection-site reactions such as redness or itching, and some people experience weight gain or swelling related to fluid shifts. Rotating injection sites can reduce local skin changes over time.
Serious adverse events may include severe hypoglycemia requiring assistance, allergic reactions (including generalized rash, trouble breathing, or swelling of the face or throat), and hypokalemia (low potassium), which can affect heart rhythm. Hyperglycemia can occur if doses are missed, insulin is not absorbed as expected, or during illness; sustained high glucose can lead to ketosis in some patients. Discuss an individualized monitoring plan with a clinician, including when to check ketones and when to seek urgent care.
Why it matters: Early recognition and treatment of hypoglycemia can prevent emergencies.
Drug Interactions and Cautions
Many medications and substances can change insulin needs by affecting glucose production, insulin sensitivity, appetite, or kidney clearance. Some drugs can increase the risk of hypoglycemia, while others can raise blood glucose and make control harder. Illness, dehydration, and changes in diet or physical activity can have similar effects and may require additional monitoring.
Examples of interaction categories clinicians often review include:
- Beta-blockers: may mask low sugar symptoms
- Corticosteroids: can raise blood glucose
- Thiazide diuretics: may increase glucose levels
- Thyroid therapy changes: can shift insulin requirements
- Alcohol: may worsen delayed hypoglycemia
Thiazolidinediones (TZDs) used with insulin can increase fluid retention in some people; clinicians watch for heart failure symptoms. Always keep an updated medication list, including over-the-counter products and supplements, and share it at each visit.
Compare With Alternatives
Rapid-acting insulin glulisine is one option for mealtime coverage. Other rapid-acting insulin analogs (such as insulin lispro or insulin aspart) and shorter-acting human regular insulin may be used in different situations, depending on meal timing needs, device preferences, and clinician experience. Regular insulin generally has a slower onset and a longer duration than rapid-acting analogs, which can change the dosing window around meals.
Device choice can also matter. Some people prefer vials and syringes for flexible dosing and supply simplicity, while others prefer pen devices for convenience. If you are comparing options, browsing hubs like Rapid Acting and Insulin Medications can help you see what categories exist.
Broader context may also help when evaluating a full diabetes regimen. You can browse Diabetes Products and Diabetes Medications to understand how insulin fits alongside other treatments, and review educational hubs like Diabetes Articles for general self-management topics. Any medication change should be paired with a monitoring plan to reduce unexpected highs or lows.
Pricing and Access
Apidra Vials require a valid prescription in most jurisdictions. Coverage and out-of-pocket responsibility vary by plan design, formulary status, and whether a pharmacy benefit or medical benefit applies. People who are without insurance may explore cash-pay pathways, but the best approach depends on local rules and individual eligibility.
As part of the referral process, prescription details may be verified with the prescriber before dispensing is arranged. Documentation requirements can include a current prescription, patient identifiers, and confirmation of the intended product form (vial versus pen). For non-medication factors that can affect daily needs, resources like Best Diet For Insulin Resistance and Type 1 Diabetes Articles can support informed conversations with a care team.
If you are comparing access pathways, informational updates may appear on the Promotions Information page, though availability and terms can change. Cross-border fulfilment considerations depend on eligibility and jurisdiction, and the dispensing pharmacy must follow applicable regulations.
Authoritative Sources
For prescribing details and official safety information, consult the current product labeling:
- DailyMed listing for insulin glulisine: National Library of Medicine drug label database
- FDA drug information resources: U.S. Food and Drug Administration drugs portal
- Diabetes standards and education: American Diabetes Association
Temperature-sensitive medicines sometimes require prompt, express, cold-chain shipping to help maintain recommended storage ranges during transit.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is insulin glulisine and what is it used for?
Insulin glulisine is a rapid-acting insulin analog used to reduce blood glucose rises that happen with meals. It is commonly prescribed for people with type 1 diabetes and for some people with type 2 diabetes who need mealtime insulin support. Because it works quickly, timing around meals and glucose monitoring are important parts of safe use. Many people use it as part of a larger plan that may include basal (long-acting) insulin, nutrition planning, and regular review of glucose data with a clinician.
How quickly should rapid-acting insulin be taken in relation to meals?
Rapid-acting insulins are generally intended for use close to meal time, but the exact timing can vary by product labeling and the individual care plan. Some labels allow dosing shortly before eating and, in certain situations, soon after starting a meal. Your prescriber’s instructions should reflect your typical meal pattern, glucose monitoring method, and risk of hypoglycemia. If meals are unpredictable or delayed, discuss safer timing strategies and a backup plan for missed or partial meals.
Can this insulin be used in an insulin pump?
Insulin glulisine is used by some people in continuous subcutaneous insulin infusion (insulin pump) therapy, but pump use requires careful setup and routine maintenance. Compatibility can depend on the pump system, infusion set materials, and the manufacturer’s instructions. People using pumps usually follow a schedule for changing infusion sets and reservoirs, and they monitor glucose closely to detect interruptions that could lead to hyperglycemia or ketosis. Any pump-setting adjustments should be made with the clinician who manages the pump regimen.
What supplies do I need to use a U-100 insulin vial safely?
A U-100 insulin vial is designed to be used with U-100 insulin syringes so that the unit markings match the insulin concentration. Using the wrong syringe type can cause significant dosing errors. You will also need new sterile needles/syringes for each injection, a sharps container for disposal, and alcohol swabs if advised by your clinic. If you use other diabetes devices (meter, CGM, pump), keep backup supplies available. Ask your pharmacist to confirm that your syringe size and unit markings fit your prescribed dosing range.
How should an opened insulin vial be stored and when should it be discarded?
Storage recommendations depend on the specific insulin product and local labeling. Unopened insulin is typically refrigerated and protected from freezing and direct heat. Once opened or first punctured, many insulin vials can be kept at controlled room temperature for a limited period, after which they should be discarded even if insulin remains. Always check the package insert for the in-use timeframe and handling details. If the solution looks cloudy, discolored, or has particles (when it should be clear), do not use it and consult a pharmacist.
What side effects need urgent medical attention while using rapid-acting insulin?
Seek urgent care for signs of a severe allergic reaction such as trouble breathing, swelling of the face or throat, or widespread rash. Severe hypoglycemia that causes confusion, seizure, loss of consciousness, or requires help from another person is also an emergency. Persistent vomiting, very high blood glucose, or symptoms suggesting ketosis (for example, abdominal pain or unusual fatigue) should be assessed promptly, especially for people with type 1 diabetes. Discuss with a clinician when to check ketones and what actions to take during illness.
What should I ask my clinician before starting or switching mealtime insulin?
Key questions include how to time doses with meals, how to adjust monitoring during exercise or illness, and what to do if you miss a dose or eat less than planned. Ask how to recognize and treat hypoglycemia, and whether you should have glucagon available. If you use a pump or CGM, confirm whether any settings need review after a change. It also helps to clarify which syringe type to use for vials, how to rotate injection sites, and when follow-up data review should occur.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
Contour Next Test Strips Practical Use And Compatibility Checks
Key Takeaways Contour Next Test Strips are single-use, in vitro diagnostic strips used with compatible glucose meters. Small details on the box and your technique can affect results. Match strip…
Why Is Ozempic So Expensive? Pricing Factors Explained
Key Takeaways Price varies because list price differs from what payers actually pay. Insurance design (deductibles, coinsurance, formularies) often drives your out-of-pocket amount. High demand and limited competition can keep…
Zepbound Pill Clarified: Injection Reality and Oral Research
Key Takeaways Current form: Zepbound is an injectable medicine, not a tablet. Search intent: “pill” usually means convenience, not a new product. Dosing language: labels use stepwise titration and maintenance…
Lancets For Blood Sugar Testing: Selection And Safety Tips
Overview Fingerstick blood glucose checks rely on small, sharp tools and consistent technique. In most home setups, a spring-loaded lancing device uses lancets to puncture skin and produce a drop…