Insulin resistance affects how your cells respond to insulin, a hormone that moves glucose into tissues. This guide explains how to cure insulin resistance safely and realistically, using nutrition, activity, sleep, and medications where appropriate. We highlight clinical concepts in plain language and add practical steps you can start today. For broader background reading, see Diabetes Articles for fundamentals and updates.
Key Takeaways
- Core drivers: Excess calories, low activity, poor sleep, and stress.
- Best levers: Whole-food diet, resistance training, and weight management.
- Medical tools: Metformin and incretin therapies can support lifestyle.
- Track progress: Waist, fasting glucose, A1C, and energy levels.
- Work with clinicians: Personalize targets and review medications regularly.
How to cure insulin resistance: What Works and Why
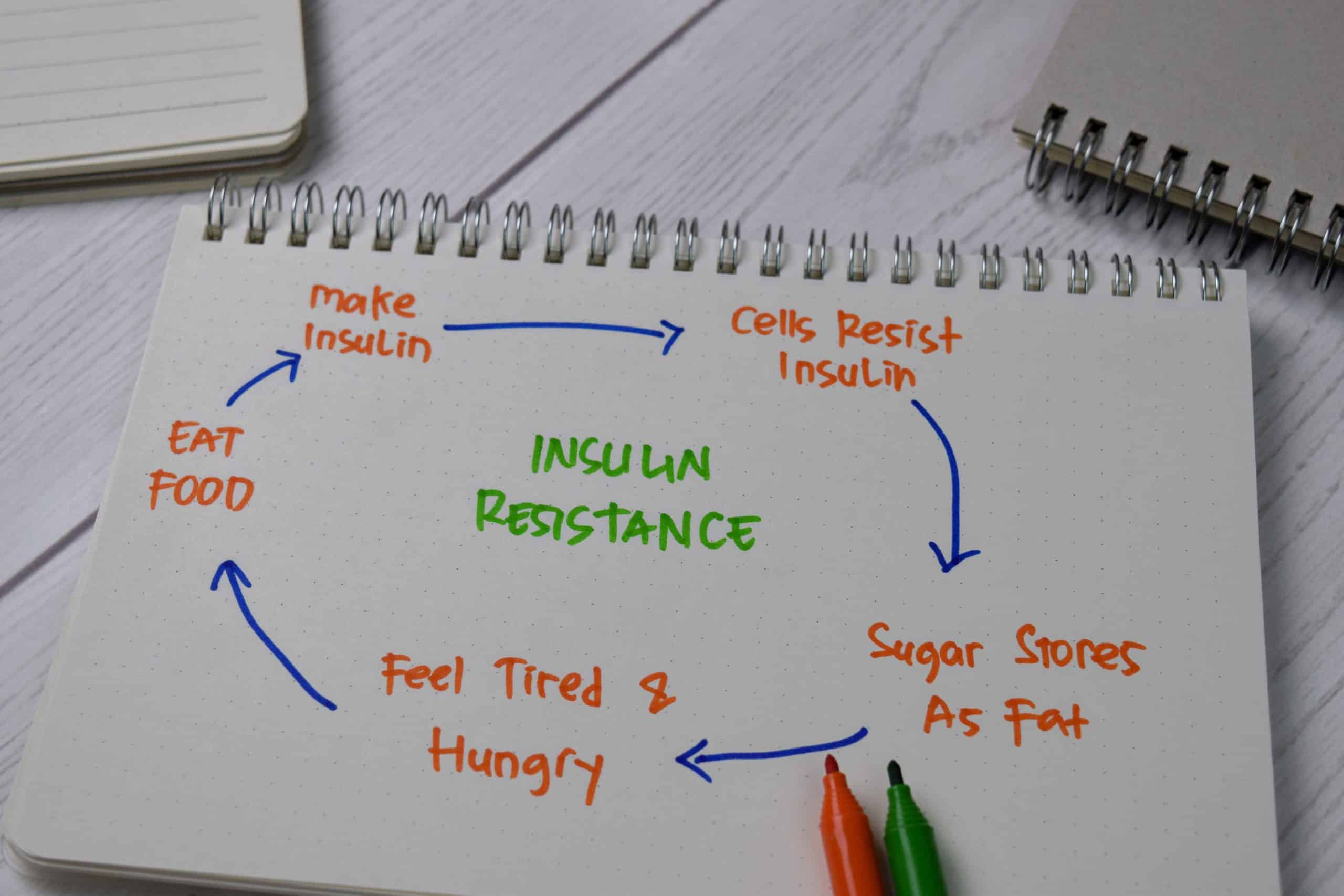
Insulin resistance means muscle, fat, and liver cells respond weakly to insulin, so the pancreas compensates by making more. Over time, this cycle raises glucose and strains beta cells in the pancreas. The result can be prediabetes and, eventually, type 2 diabetes. Breaking this loop requires lowering insulin demand and improving tissue sensitivity.
Most people improve by addressing energy balance and activity. Losing even 5–10% of body weight can reduce liver fat (hepatic steatosis), ease inflammation, and restore insulin signaling. Resistance training boosts muscle glucose uptake by increasing GLUT4 transporters, while regular aerobic work improves mitochondrial function. Sleep hygiene and stress reduction help normalize cortisol, which otherwise promotes insulin resistance.
What Is Insulin Resistance (and Why It Matters)
Insulin resistance is a metabolic state where insulin’s signal to move glucose into cells is blunted. Clinically, this can coexist with normal glucose for years, thanks to higher insulin output (hyperinsulinemia). Eventually, the pancreas cannot keep up, and fasting glucose rises. That transition marks higher cardiometabolic risk.
Why this matters: insulin resistance links to nonalcoholic fatty liver disease, high triglycerides, hypertension, and polycystic ovary syndrome (PCOS). It also raises long-term risks for cardiovascular disease. Understanding the biology supports better choices around diet quality, movement, and sleep schedules. Early action reduces the chance of progression and medication escalation later.
What Causes Insulin Resistance
Multiple factors contribute, but excess caloric intake and low physical activity dominate. Genetics, aging, sleep restriction, and chronic stress add to the load. Ectopic fat in the liver and muscle interferes with insulin signaling, while inflammatory cytokines worsen cellular responses. Practical changes target these drivers in parallel for the best effect.
To address root causes, identify weight-promoting patterns, such as sugary beverages, large late dinners, or frequent takeout. Then add structure around meals and movement. Discuss any endocrine conditions that may contribute to metabolism. For a broader comparison between related metabolic states, see Insulin Resistance vs. Diabetes for context on progression risks and markers.
Some people ask directly about what causes insulin resistance because understanding drivers shapes early actions. Common culprits include energy-dense foods, prolonged sitting, and poor sleep hygiene. These can be modified without extreme measures or restrictive rules.
Diagnosing and Monitoring Progress
No single office test “diagnoses” insulin resistance in routine practice. Clinicians infer it from patterns: waist circumference, fasting glucose, A1C (glycated hemoglobin), fasting triglycerides, HDL cholesterol, and sometimes fasting insulin. The oral glucose tolerance test (OGTT) clarifies how your body handles a defined glucose load. For authoritative basics on insulin resistance and prediabetes, review the NIDDK overview, which summarizes mechanisms and risks in plain language.
At home, track morning weight, waist at the navel, and fasting glucose if you use a meter. Some people try continuous glucose monitors (CGMs) to observe patterns, especially around meals and sleep. Repeat A1C and lipids as advised by your clinician. For structured reading around type 2 screening and follow-up, browse Type 2 Diabetes for diagnostic pathways and treatment updates.
Nutrition Strategy and Meal Planning
A well-designed insulin resistance diet emphasizes whole foods, adequate protein, and high-fiber carbohydrates. Choose minimally processed options: vegetables, legumes, whole grains, lean proteins, and unsweetened dairy or fortified alternatives. Replace refined carbs and sugary drinks with water, tea, or coffee without added sugar. This reduces insulin demand and supports satiety.
Prioritize protein at each meal, around a palm-sized serving, and include fiber-rich sides to slow glucose absorption. Time meals consistently and consider an earlier dinner when possible. If you prefer plant-forward patterns, build meals around beans, lentils, tofu, tempeh, and nuts. For practical menus and portions, see Best Diet for Insulin Resistance, which organizes foods by meal type for quick planning.
Tip: Stock a short list of go-to meals. Repeating simple breakfasts and lunches reduces decision fatigue and improves adherence.
Exercise, Sleep, and Stress
Activity improves glucose uptake immediately and increases insulin sensitivity over days to weeks. Aim for a blend: 2–3 days per week of resistance training and 150 minutes per week of moderate aerobic work. Spread movement across the week. Short walks after meals help flatten post-meal glucose. The ADA’s yearly standards outline exercise targets and safety considerations in clinical guidelines.
Sleep seven to nine hours nightly and keep consistent bed and wake times. Reduce evening caffeine and screens. Use brief breathing exercises, stretching, or mindfulness to manage stress. These behaviors make it easier to maintain diet and movement changes. If weight management is your immediate goal, read Lose Weight With Insulin Resistance for stepwise tools you can apply next week.
People often ask how to reverse insulin resistance using training. The most reliable approach combines progressive strength work with regular brisk walking or low-impact cardio. Together, these reduce visceral adiposity and improve insulin signaling.
Medications and Adjuncts
Lifestyle remains foundational, but medications may support metabolic control. Many clinicians start metformin (an insulin sensitizer) for prediabetes and type 2, given its safety profile and low cost. When diet and exercise are already in motion, metformin for insulin resistance can help lower hepatic glucose production. Always discuss benefits and risks for your situation.
Newer agents can complement the plan. SGLT2 inhibitors promote urinary glucose excretion and may aid weight control. For a therapy overview, see Dapagliflozin when exploring SGLT2 options and indications in practice. Combination regimens sometimes include DPP-4 inhibitors with metformin; review Janumet XR for a sense of how fixed-dose combinations are structured and when they may be considered. For prescribing considerations and safety details, consult the FDA label, which summarizes indications and cautions for metformin products.
Women’s Health Signals
Hormonal patterns influence metabolic function. In PCOS, elevated androgens and irregular ovulation often correlate with insulin resistance. Symptoms can include irregular cycles, acne, scalp hair thinning, and weight gain around the abdomen. Addressing sleep, diet quality, and strength training helps many people with PCOS improve metabolic markers and energy levels.
Clinicians consider life stage, contraception, and pregnancy plans when tailoring therapy. Some find that antiandrogen effects of weight loss and improved insulin sensitivity reduce cycle irregularity. If you want to compare mechanisms, see Insulin Resistance vs. Insulin Deficiency for a clearer picture of where the problem lies in each condition. Many readers search for insulin resistance symptoms in females because early recognition guides timely intervention.
Is It Working? Signs and Timelines
You can monitor change across several dimensions. Waist circumference trending downward suggests less visceral fat. Fasting glucose stabilizes, and post-meal spikes become smaller. Energy and satiety often improve. These shifts usually precede large changes in A1C because A1C reflects roughly three months of glycemia. For context on therapies affecting weight, scan GLP-1 Weight-Loss Drugs, which outlines how these agents modify appetite and glucose handling.
Common signs insulin resistance is reversing include smaller morning glucose swings, lower triglycerides, and improved sleep quality. Avoid exact timelines, because rates vary by baseline weight, adherence, medications, and sleep. Objective markers plus how you feel day to day give the best signal. Routine follow-up with your clinician keeps targets realistic and safe.
Supplements and Natural Supports
Some supplements may support insulin sensitivity as part of a broader plan. Magnesium, omega-3s, and berberine are frequently studied; quality varies, and effects are modest compared with diet and exercise. Discuss potential interactions with your clinician, especially if you take glucose-lowering medications or anticoagulants. Food-first strategies remain the backbone of improvement.
Whole-food choices often deliver similar benefits with fewer risks. For examples, berries and legumes provide fiber and polyphenols that aid glucose control; learn practical ways to use them in Berries for Diabetes and Beans and Diabetes, both of which summarize preparation tips and meal ideas. If you choose supplements, select third-party tested products and monitor labs during use.
Putting It Together: A Simple Weekly Framework
Start with predictable meals and scheduled activity. Build a repeating breakfast and lunch, then rotate two balanced dinners. Schedule three resistance sessions on nonconsecutive days and add short, brisk walks after larger meals. Keep a short checklist: protein source, fiber side, colorful produce, and a healthy fat.
Plan two weekly check-ins. First, review weight, waist, and energy. Second, assess one behavior to improve next week, such as going to bed 30 minutes earlier or preparing snacks at home. If you want deeper menu structure and grocery lists, see Insulin Resistance Diet, which organizes choices by food groups and weekly patterns.
Note: Rapid, extreme changes are rarely sustainable. Aim for steady progress and revisit your plan monthly.
This content is for informational purposes only and is not a substitute for professional medical advice.