Key Takeaways
- Silent early damage: albumin in urine may appear before symptoms.
- Stage by eGFR and albumin-to-creatinine ratio for clarity.
- Control glucose, blood pressure, and lipids to slow decline.
- ACE inhibitors, ARBs, and SGLT2 inhibitors can reduce risk.
- Accurate coding supports tracking and multidisciplinary care.
Many people first learn about diabetic nephropathy during routine labs, not from symptoms. Early identification matters because small changes in albumin or estimated GFR can guide timely care. Managing blood pressure, glucose, and cardiovascular risks together offers the best protection for long-term kidney health.
What Is Diabetic Nephropathy?
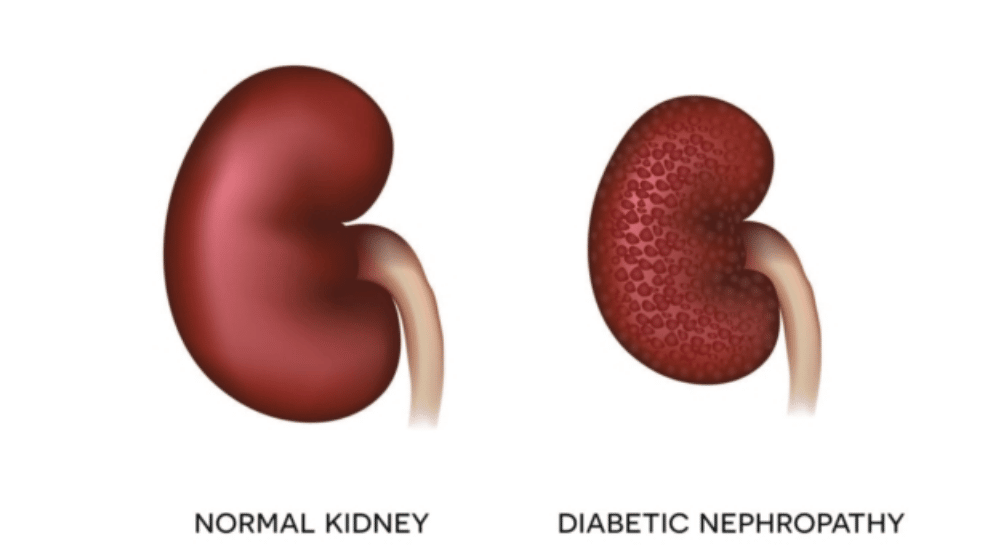
Diabetic kidney disease (DKD) is kidney damage caused by long-standing diabetes. Clinicians often call it diabetic nephropathy, and both terms appear in practice and literature. High blood glucose and high blood pressure injure glomeruli (the kidney’s filters), leading to protein leakage and gradual decline in filtration. Over time, scarring disrupts function, and the risk of cardiovascular events rises.
Some programs use the term DKD to emphasize that many pathways contribute to kidney injury in diabetes. For a broader comparison of terminology and overlap, see Diabetic Kidney Disease for context and definitions. The related overview on Diabetes and Kidney Damage explains how hyperglycemia, hypertension, and inflammation interact, which helps you understand prevention choices.
Early Signs, Presentation, and Symptoms
Early disease rarely causes noticeable symptoms. The first signal is usually a small increase in urinary albumin, detected on a urine albumin-to-creatinine ratio (UACR). As kidney damage progresses, patients may notice ankle swelling, foamy urine, nighttime urination, or rising blood pressure. Fatigue and appetite changes can appear later and are not specific to kidney disease, so routine screening remains crucial.
Clinicians often describe diabetic nephropathy symptoms in terms of albuminuria and declining eGFR rather than pain or discomfort. For those documenting chart details, microalbuminuria icd-10 coding can support problem-list accuracy and trend tracking. For a broader patient-focused summary of complications, the brief guide in Diabetes and Kidney Damage provides useful context and self-care priorities.
Staging and Pathology
Staging clarifies disease severity and informs follow-up. Many teams describe diabetic nephropathy stages using two axes: glomerular filtration (G1–G5 by eGFR) and albuminuria (A1–A3 by UACR). For example, a person with eGFR 75 mL/min/1.73 m² and moderately increased albuminuria falls in early CKD, while someone with eGFR 25 and severe albuminuria needs close multidisciplinary care. Consistent staging helps coordinate decisions on medications, imaging, and specialist referral.
Histologic changes accumulate over time. Characteristic features can include mesangial expansion, thickened glomerular basement membrane, and nodular glomerulosclerosis (Kimmelstiel–Wilson lesions). These pathologic changes align with progressive albumin leakage and declining filtration. Staging by eGFR and albuminuria does not require biopsy, but pathology explains why pressure and glucose control matter.
Pathophysiology and Histology
Chronic hyperglycemia drives oxidative stress, advanced glycation end-product formation, and intraglomerular hypertension. The renin–angiotensin–aldosterone system (RAAS) amplifies glomerular pressure, while inflammatory pathways and fibrosis worsen structural injury. Over time, afferent and efferent arteriolar tone changes keep pressure high within the glomerulus, pushing albumin into the urine. Mesangial matrix expansion decreases filtration surface area, and tubulointerstitial fibrosis limits recovery potential. This pathophysiologic cascade explains why therapies that reduce glomerular pressure and inflammation can slow progression.
Diagnosis and Monitoring
Screening usually includes annual UACR and eGFR, with more frequent testing when abnormalities appear. A diagnosis is supported by persistent albuminuria on at least two of three tests over three to six months, along with compatible clinical context. Blood pressure assessments, electrolytes, and lipid panels help define overall risk. Eye exams and neuropathy screening often run in parallel, since microvascular complications frequently cluster.
Practice standards recommend early detection and risk reduction in diabetes care. For screening intervals and referral criteria, see the ADA Standards of Care on chronic kidney disease and diabetes (opens in a new tab) from an authoritative source, the American Diabetes Association ADA Standards of Care. For a broader kidney focus across conditions, the U.S. National Institute of Diabetes and Digestive and Kidney Diseases offers accessible materials; review their guidance on diabetic kidney disease for patient education and clinician handouts NIDDK resources. When confirming diabetic nephropathy diagnosis, document other causes of CKD if suspected, using history, urinalysis, and imaging where appropriate.
Treatment and Risk Reduction
Care focuses on protecting the kidneys and the heart. Lifestyle measures include sodium moderation, individualized nutrition, physical activity, and avoiding nephrotoxic drugs when possible. Blood pressure control is foundational; ACE inhibitors or ARBs are commonly first-line for albuminuric disease. Examples include Irbesartan and Losartan, which are discussed here to illustrate RAAS blockade in practice. ACE inhibitors such as Captopril may be used when appropriate. Diuretics like Furosemide Injection can help manage volume in edema.
Glucose management supports kidney protection, though targets remain individualized. SGLT2 inhibitors reduce albuminuria and slow CKD progression in many patients with diabetes. For a concise summary of the renal evidence, see Farxiga and Kidney Health, which outlines outcome data and eligibility considerations Farxiga and Kidney Health. Multi-morbidity care includes lipid management and vaccinations. For guideline-level synthesis across therapies, the kidney–diabetes guideline from KDIGO summarizes recommended strategies and thresholds; consult the 2022 KDIGO document for detailed algorithms KDIGO diabetes in CKD. Many clinicians describe these steps collectively as diabetic nephropathy treatment, but plans should be personalized and periodically reviewed.
Coding and Documentation Basics
Accurate documentation helps track disease stage and guide benefits or referrals. Many records use a combination of diabetes codes and CKD staging codes. A commonly used label in charts is type 2 diabetes mellitus with diabetic nephropathy icd-10, which is typically combined with a CKD stage code to reflect severity. Include the current eGFR and UACR values in notes to align the diagnostic code with the patient’s status.
Use consistent terminology when albuminuria is present, and record changes over time. Some practices add problem-list entries for hypertension and dyslipidemia to reflect the cardiovascular risk bundle. For a structured view of related material and trends, you can scan Diabetes Articles for recent updates and practical explainers Diabetes Articles. When prescribing or reconciling therapies, your team may also review medication references under Diabetes Medications to ensure class coverage is complete Diabetes Medications.
Can Kidney Damage Be Reversed?
Some changes can improve, especially early albuminuria, with intensive risk-factor management. SGLT2 inhibitors, RAAS blockers, and lifestyle measures can reduce albumin levels and slow decline in filtration. However, advanced scarring is less likely to reverse, and sustained control becomes the priority. Ask teams to coordinate blood pressure goals, glucose targets, and follow-up testing intervals, which together shape long-term outcomes.
People often search for how to reverse kidney damage from diabetes and get mixed messages. A practical approach focuses on small, measurable steps: reduce sodium intake, reach individualized A1C and blood pressure targets, and monitor UACR and eGFR regularly. For data-based guidance on combining therapies, the ADA and KDIGO provide complementary recommendations; see the preceding links to their materials. When edema or resistant hypertension emerges, diuretics and specialist input may add benefit.
Living With DKD: Practical Tips
Work with your care team to set priorities you can maintain. Many people start with blood pressure, using home monitoring to track trends. If edema occurs, daily weights can help detect fluid shifts early. Avoid nonsteroidal anti-inflammatory drugs when possible, and confirm all over-the-counter supplements with your clinician, since some can affect kidney function or interact with therapies.
Education helps people anticipate decisions and spot early change. You can review Diabetic Kidney Disease for deeper background on risk and terminology Diabetic Kidney Disease. For a concise, action-focused overview, the campaign piece in National Kidney Month offers reminders you can adapt to everyday habits National Kidney Month. When considering insulin strategies alongside kidney care, primers such as Common Diabetes Medications can clarify classes and uses without replacing individual advice Common Diabetes Medications.
Recap
Early detection and steady risk reduction offer the best path to protect kidney function. Use albuminuria and eGFR together to stage disease, document progress, and coordinate therapies. Reinforce lifestyle steps that you can sustain, while regularly reviewing medications that protect the kidneys and heart. The overall plan works best when diabetes, blood pressure, and lipids are addressed together.
For further reading, see Diabetes and Kidney Damage for a quick overview of complications and prevention strategies Diabetes and Kidney Damage. If medication choices are being considered, your team can consult class examples such as Irbesartan or Losartan to understand RAAS options in context. These resources do not replace individualized medical advice or shared decision-making.
Note: Terms like DKD and diabetic nephropathy often overlap in practice. Health systems may prefer one term for consistency, but the core prevention and monitoring steps remain the same.
This content is for informational purposes only and is not a substitute for professional medical advice.