A diabetes attack can develop quickly and feel overwhelming. Understanding the patterns, triggers, and emergency steps helps you act fast and reduce harm. This guide uses clear language and clinical terms to make quick decisions easier.
Key Takeaways
- Know early warning signs and severe red flags.
- Treat low and high glucose differently and promptly.
- Check ketones during illness or persistent high readings.
- Create an action plan and keep rescue tools ready.
What Is a Diabetes Attack?
People use this non-medical phrase to describe acute, symptomatic glucose crises. Clinicians usually classify these as hypoglycemia (low blood glucose), hyperglycemia (high blood glucose), or metabolic emergencies such as diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). Each has distinct mechanisms, timelines, and treatments.
Hypoglycemia occurs when glucose falls below safe thresholds, depriving the brain of fuel and impairing judgment. Hyperglycemia rises when insulin is insufficient or ineffective, creating dehydration and electrolyte shifts. DKA and HHS reflect more severe metabolic derangements that can progress to coma without urgent care. Recognizing patterns early limits complications and hospitalizations.
Recognizing Early and Severe Symptoms
Patterns vary by person and medications, but some cues are common. Early neuroglycopenic signs include difficulty focusing, blurry vision, irritability, and headache. Autonomic responses may cause sweating, tremor, palpitations, and intense hunger. Keep a written list of your typical cues for quick reference.
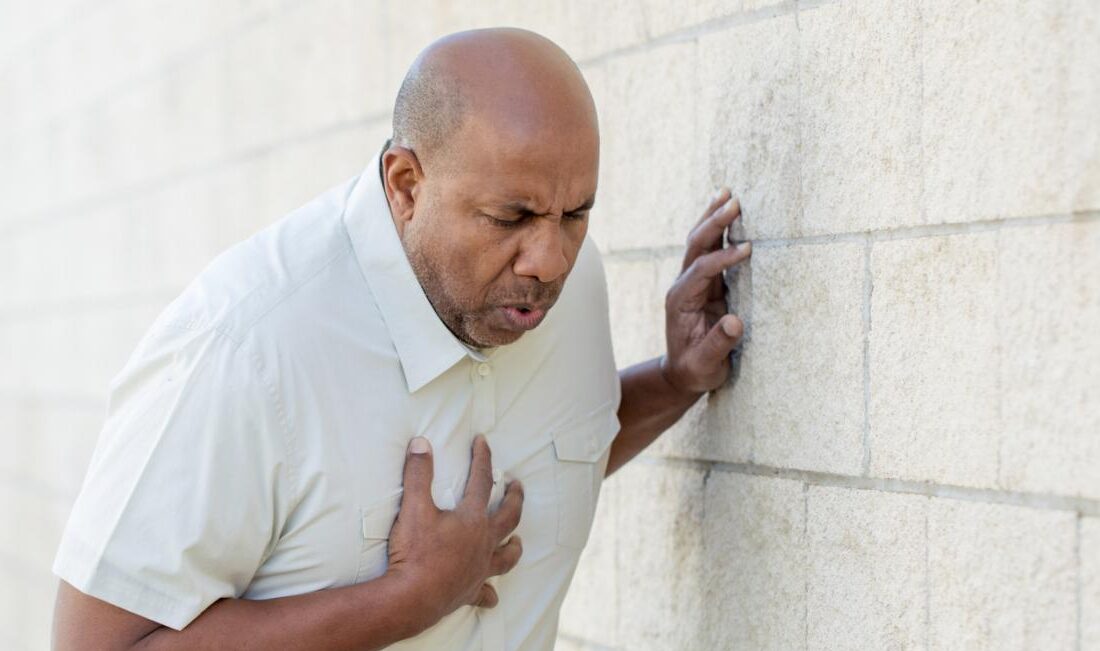
Severe features may include confusion, slurred speech, vomiting, chest pain, or seizure. These can overlap, so confirm with a meter or continuous monitor when possible. Knowing classic diabetes attack symptoms improves confidence and helps caregivers intervene appropriately. When in doubt, test and treat based on the reading, not assumptions.
Low Blood Sugar Emergencies (Hypoglycemia)
Low blood glucose can develop within minutes, especially after excess insulin, skipped meals, or unexpected exertion. Typical hypoglycemia emergency symptoms include shakiness, sweating, dizziness, confusion, and sometimes behavior changes. In severe cases, people may become unresponsive. Acting rapidly protects the brain.
Use the 15-15 rule: take 15 grams of fast carbohydrate (e.g., glucose tablets, regular soda), then recheck in 15 minutes. Repeat until above your safe threshold, then eat a snack with protein and carbs. If swallowing is unsafe or the person is unconscious, use glucagon if available and call emergency services. The American Diabetes Association describes standard hypoglycemia recognition and treatment in accessible terms (ADA guidance on low blood glucose).
If you use combination therapy, medication selection influences risk. For background on a metformin plus SGLT2 option and its mechanism, see Synjardy How It Works for context on how different agents affect glucose.
High Blood Sugar Emergencies (Hyperglycemia)
High glucose builds more gradually, but can accelerate with missed insulin, illness, or dehydration. Early symptoms include excessive thirst, frequent urination, fatigue, and blurred vision. With ongoing elevation, nausea, abdominal pain, rapid breathing, and fruity breath may appear, suggesting ketosis or acidosis.
Key hyperglycemia emergency symptoms include persistent readings above your target range with dehydration and worsening malaise. People on rapid-acting insulin may use correction doses per their plan. For reference on a fast insulin option, see the NovoRapid Cartridge page for product characteristics that inform timing and action.
Severe hyperglycemia can cause dangerous fluid shifts. The U.S. National Institutes of Health provides a clear overview of DKA, including hallmark signs and when urgent care is needed (MedlinePlus DKA overview).
DKA, HHS, and Confusion With Hypoglycemia
DKA typically occurs with significant insulin deficiency, often in type 1 diabetes but also in insulin-deficient type 2. It features high glucose, ketones, acidosis, and dehydration. HHS often appears in older adults with type 2, showing very high glucose and severe dehydration, typically without marked acidosis. Both can progress to altered consciousness.
Because some early symptoms overlap, people sometimes wonder about dka vs hypoglycemia when they feel unwell. Objective data resolves uncertainty: use fingerstick glucose and, if high, check blood or urine ketones. During intercurrent illness such as pancreatitis, risks may rise; for background on those links, see Pancreatitis and Diabetes to understand how inflammation can disrupt metabolic control.
First Aid and Action Steps
Use structured steps to minimize errors under stress. First, test blood glucose or review your CGM reading and trend arrows. Next, act based on the number and symptoms. Treat lows with fast carbs; treat highs with hydration and your prescribed correction strategy if appropriate.
If you are unsure or cannot test, treat as low rather than wait. Teach family members what to do during a diabetes attack so they can offer timely help. Keep a glucagon kit accessible, and rehearse where it is stored. For broader therapy comparisons that may influence day-to-day risk of hypoglycemia, see Rybelsus vs Metformin for an overview of oral options and expected effects.
Tip: Create a wallet card listing your typical low and high symptoms, your target glucose range, and emergency contacts. Share this with caregivers and coworkers.
Monitoring, Ketones, and Sick-Day Rules
Illness, dehydration, and missed insulin can accelerate ketosis, especially in type 1 diabetes. Check ketones whenever glucose remains high despite corrections, during vomiting, or when you feel acutely unwell. Blood ketone meters provide faster, more precise data than urine strips, which can lag behind current status.
Learn how to check ketones for diabetes and record thresholds in your action plan. During sick days, increase monitoring frequency, maintain hydration, and continue basal insulin unless your clinician advises otherwise. The Centers for Disease Control and Prevention outlines practical sick-day planning steps, including hydration, carbohydrate intake, and monitoring frequency (CDC sick-day guidance).
People using GLP-1 medicines sometimes adjust intake during gastrointestinal illness. For travel and routine planning ideas that keep doses on schedule, see Travel With Ozempic for practical preparation tips. For a broader library of education pieces, browse our Diabetes Articles collection to find condition-focused guides.
When to Seek Emergency Care
Some situations require immediate professional help. Call emergency services for unconsciousness, seizures, suspected stroke-like symptoms, chest pain, severe dehydration, or relentless vomiting. If ketones are moderate to high and not improving with home measures, urgent evaluation is prudent. Children, older adults, and pregnant individuals may decompensate faster.
Use the phrase when to go to er for diabetes as a mental checklist: altered consciousness, breathing difficulties, persistent high ketones, or inability to keep fluids down. Trust your instincts and escalate early if self-care is failing. For ongoing medication education and supply planning, the Diabetes Medications category provides product families to review with your clinician. You can also explore Trulicity Pros and Cons for a balanced look at once-weekly options and their side-effect profiles.
Prevention: Routines, Tools, and Support
Prevention starts with consistent routines: regular meals, accurate carbohydrate counting, and matching insulin to food and activity. Calibrate correction factors with your care team and revisit them after weight change, new medications, or illness. Dehydration amplifies hyperglycemia, so sip fluids steadily during hot weather and exercise.
Technology can help. Continuous glucose monitor alarms provide early warnings before symptoms arise. Set cautious alerts overnight and during travel to reduce risk. If you take metformin, extended-release options may improve tolerability; see Glumetza for a reference profile you can discuss with your clinician. For emerging oral incretin therapies, Orforglipron vs Rybelsus summarizes evolving options and how they fit into modern care.
Some individuals ultimately need insulin intensification to prevent morning or meal spikes. If you are evaluating rapid-acting regimens, coordinate with your team to tailor timing, doses, and correction strategy. To understand broader GLP-1 benefits relevant to cardiometabolic risk, see Mounjaro Heart Benefits for context on outcomes beyond glucose numbers.
Recap
Acute glucose crises are manageable with clear steps and preparation. Use monitoring data, treat lows and highs decisively, and escalate care early when needed. Build a simple action plan, stock rescue tools, and share your plan with people around you. Small habits and timely checks prevent most emergencies and protect long-term health.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.