The Apidra SoloStar Pen is a prefilled device for mealtime insulin delivery. It holds a rapid analog formulation designed to reduce post-meal glucose rises. This guide explains how it works, when to use it, and what safety factors to consider. It also covers technique, comparisons with similar products, and practical handling tips.
Key Takeaways
- Mealtime coverage: fast onset for post-meal spikes.
- Use technique: attach needle, prime, inject correctly.
- Dose guidance: individual, provider-directed adjustments.
- Safety first: watch for low glucose and site reactions.
- Storage matters: follow in-use and unopened rules.
What It Is and How It Works
This formulation contains a rapid-acting analog engineered for quick absorption from subcutaneous tissue. It begins working within minutes and helps limit meal-related glucose excursions. The active analog binds insulin receptors and supports glucose uptake into muscle and fat, while suppressing hepatic glucose production. This combination supports postprandial control when used as part of a comprehensive plan.
Pharmacology and clinical use recommendations are described in official labeling; for detailed receptor and kinetic data, see the FDA prescribing information for mealtime insulin glulisine. In day-to-day care, clinicians align dose timing with meal size, carbohydrate content, and recent glucose readings. That approach helps reduce variability and lowers hypoglycemia risk when combined with monitoring.
For a structured overview tailored to this analog’s role, see Understanding Apidra Insulin for context on mealtime control strategies.
In clinical shorthand, the product’s apidra mechanism of action centers on rapid receptor engagement and predictable tissue uptake. That profile supports flexible dose timing close to meals in many treatment plans.
Indications and Therapeutic Role
This analog is indicated for adults with type 1 or type 2 diabetes who require prandial insulin. It is often paired with basal insulin to address both fasting and post-meal glucose. Clinicians may also use it in correction dosing to address unexpected hyperglycemia. Patient-specific factors such as kidney function, injection technique, and meal timing influence final decisions.
Guideline frameworks help position mealtime analogs in therapy; see the American Diabetes Association’s Standards of Care for evidence-based use guidance. Within those frameworks, the specific apidra indication is mealtime control as part of a broader insulin regimen. Selection among rapid analogs often comes down to availability, device preferences, and response.
For additional background by condition, browse Type 1 Diabetes resources for foundational insulin education.
Onset, Peak, and Duration
This mealtime analog is formulated to act quickly after subcutaneous injection. It typically begins reducing glucose within minutes, peaks during early postprandial periods, and tapers over a few hours. That profile allows dose timing near the start of a meal in many cases. Individual factors, such as injection site and local blood flow, can shift timing slightly.
Understanding expected time course supports safer correction dosing and meal planning. The practical window avoids stacking doses too close together. Clinicians often emphasize consistent timing and careful tracking of food intake. To anchor expectations, the apidra duration of action is measured in hours rather than all-day coverage.
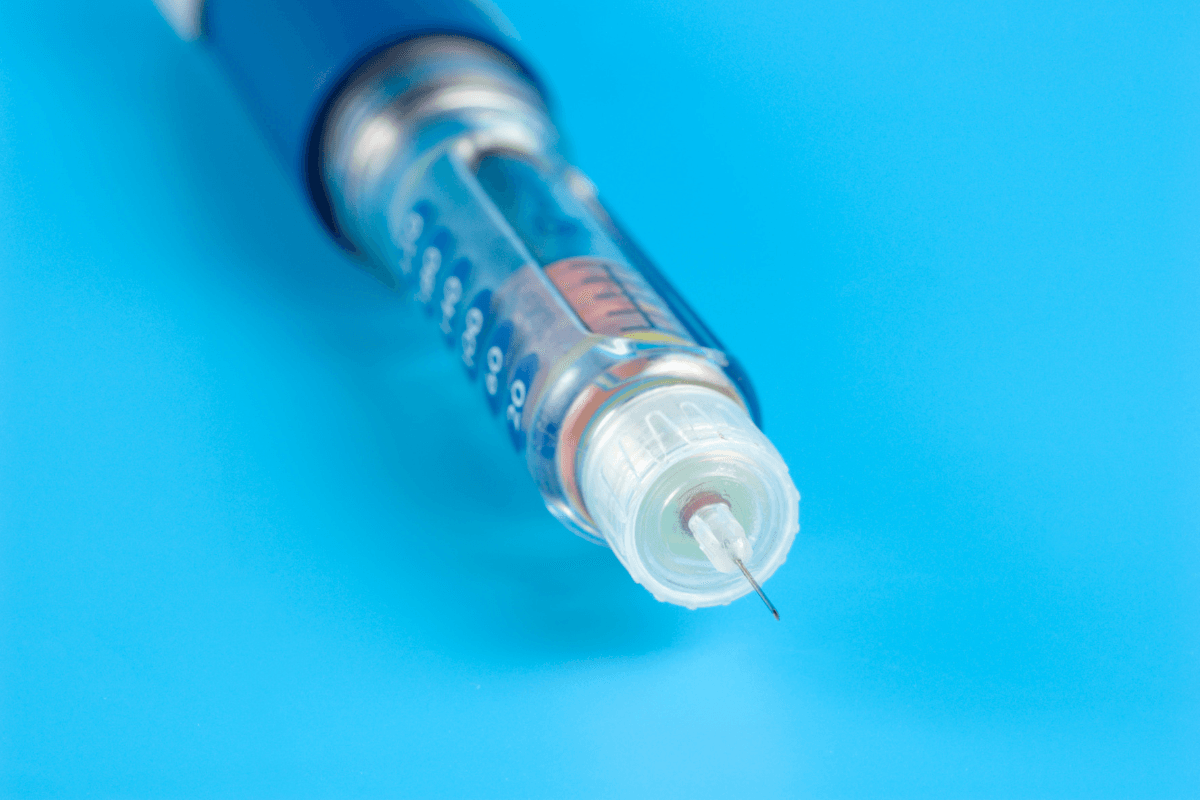
Using the Apidra SoloStar Pen
Before each dose, check the solution through the viewing window; it should be clear and colorless. Wash hands, attach a new needle, and prime the device by dialing a small amount and pressing until a steady stream appears. Priming helps remove air and confirms flow. Next, dial the dose as directed by your care team.
Choose an approved injection site, clean the skin, insert the needle at the recommended angle, then deliver the dose by pressing and holding the button. Keep the needle in place for several seconds to ensure full delivery. Remove and safely discard the needle immediately after each use. For a practical walkthrough on dose timing and intended use cases, see Apidra SoloStar Pen Uses for device-specific tips.
For device specifications and compatible needles, see Apidra SoloStar Pens to review format and strengths. When vial-based dosing is needed, compare with Apidra insulin vials to understand presentation differences.
Dosing Principles and Adjustments
Dosing is individualized and guided by your clinician. It is typically aligned with anticipated carbohydrate intake, recent glucose values, and activity plans. Some regimens use carbohydrate ratios and correction factors to translate food and readings into dose units. Others use set doses with meal-size adjustments. Always follow the plan provided by your care team.
Changes in weight, renal function, or daily routines may require reevaluation. When comparing alternatives or considering device changes, review formulation, onset, and delivery differences. For perspective on options and naming, see Apidra Generic Name And Alternatives to understand therapeutic interchange considerations. If switching mealtime products or devices, consult your prescriber to avoid unintended variability in response. The term apidra dosage always refers to a personalized amount.
Carbohydrate Ratios and Corrections
Many patients use a carbohydrate ratio to estimate units needed per gram of carbohydrates. A separate correction factor may be applied to address a high pre-meal reading. These tools work best with consistent tracking and a reliable meter or CGM. Clinicians typically adjust ratios over time based on logs of meals, readings, and hypoglycemia episodes. Structured records help identify trends and refine dosing safely.
For additional comparisons during switches, see the Apidra vs. Humalog overview, which outlines similarities and differences in action.
Administration Sites and Technique
Subcutaneous injection in the abdomen, thigh, upper arm, or buttock is standard. Rotate sites to reduce lipodystrophy and maintain predictable absorption. Keep injections at least a finger-width apart from previous sites. Avoid areas with redness, scars, or inflammation. Good technique improves comfort and helps maintain steady timing of action.
Using the correct needle length and angle may improve delivery reliability. Needle changes with each dose help reduce infection risk and leakage. For those who alternate between pens and vials, carefully confirm the correct device steps before dosing. When syringes are required for vial use, review BD Ultra-Fine II Syringes for gauge and length options. The recommended apidra route of administration is subcutaneous injection per labeling.
Side Effects and Precautions
Low blood glucose is the most common risk. Symptoms may include shakiness, sweating, confusion, or palpitations. Keep a rapid source of glucose available and follow your care team’s hypoglycemia plan. Injection-site reactions, such as redness or swelling, can occur and usually resolve without treatment. Rotating sites and proper technique help reduce local effects.
Certain medications, changes in kidney function, or illnesses can shift insulin requirements. Work with your clinician to reassess dosing during acute illness or significant routine changes. For safety details and recognized adverse events, the official product label provides comprehensive information. For a deeper side-effect breakdown, see Apidra SoloStar Pen Side Effects to review practical management tips. The phrase apidra side effects also covers injection-site reactions and allergic responses.
Comparisons with Other Mealtime Insulins
Mealtime analogs share a broadly similar timing profile but differ in device options and formulation details. Patient preference, familiarity, and insurance coverage often influence selection. When considering a switch, review onset, peak, device usability, and your data logs with a clinician. Comparable control can often be achieved, but dose adjustments may be needed during transitions.
For head-to-head insights on selection, the guide on Apidra vs. Humalog summarizes practical differences in use. Parents and pediatric teams may also consider device formats like the Humalog KwikPen Junior when size and increments matter. For background on aspart formulations, see Novolog Insulin Aspart Uses for a related rapid analog. Within this section, the comparison phrase apidra vs humalog highlights a common decision point.
Storage, Stability, and Handling
Before first use, follow the storage conditions on the label and keep pens protected from extreme temperatures. Once in use, pens are typically stored at room temperature within labeled time limits. Avoid heat, freezing, and direct sunlight. Discard pens that are expired, frozen, or show cloudy/particulate solution. Always remove the needle after dosing to reduce leakage and contamination.
When travel or daily routines change, plan how you will maintain temperature control and carry backup supplies. Keep a written dosing plan and your clinician’s contact information accessible. If your regimen sometimes requires vials, review NovoRapid Vials to understand how vial handling differs from prefilled pens. For curated topics across conditions and therapies, explore the Diabetes article archive for storage and technique primers.
When Alternatives or Add-Ons Are Considered
Most mealtime analogs can meet postprandial needs when used correctly. Device preference, response patterns, or supply access may prompt consideration of alternatives. In such cases, clinicians review history, hypoglycemia patterns, and lifestyle needs before switching. Short trial periods with careful logging can support a safe transition.
When integrating with a basal insulin strategy, timing and dose balance matter. Some regimens use different basals or fixed-ratio combinations, depending on goals. For multi-drug pen options that streamline care, see Soliqua SoloStar Pen for dual-action background. Device usability and predictability often drive durable choices. If comparing pen platforms, you can also review Humalog KwikPen to understand dial features and increments.
Recap
This mealtime insulin provides rapid coverage when timed around meals. Safe, effective use depends on good technique, individualized dosing, and regular monitoring. Understanding kinetics, side effects, and alternatives supports confident day-to-day management. Keep communication open with your care team for adjustments over time.
This content is for informational purposes only and is not a substitute for professional medical advice.