Knowing how Basal vs Bolus insulin work together can help you discuss safer, steadier glucose control with your care team. Basal insulin provides background coverage between meals and overnight. Bolus insulin addresses mealtime rises and corrections. This guide explains core concepts, typical ratio ranges, weight-based starting frameworks, and how different insulin types fit into daily regimens. It uses plain language alongside clinical terms, so you can recognize options and ask clearer questions.
Key Takeaways
- Two roles, one plan: basal covers background needs; bolus covers meals.
- Ratios vary by person and time; reassess when patterns change.
- Weight-based frameworks guide starts, not final individualized doses.
- Insulin types differ in onset, peak, and duration; match to needs.
- Use structured tracking, cautious adjustments, and professional guidance.
Basal vs Bolus: What Each Insulin Does
Basal insulin delivers a steady, low-level supply that limits hepatic glucose output between meals and during sleep. In plain terms, it keeps background glucose stable when you are not eating. Clinically, this is long-acting or intermediate insulin, dosed once or twice daily depending on the product and response.
Bolus insulin (prandial insulin) covers carbohydrate intake at meals and corrects high readings. Fast onset and shorter action help match post-meal glucose rises. Together, basal and bolus doses form the basal-bolus regimen, which aims to mimic physiologic secretion while respecting each person’s schedule and sensitivity.
Dosing Concepts and Ratios
Many plans start with a flexible split between background and mealtime doses. The basal vs bolus insulin ratio often falls near a balanced allocation, though needs vary by age, activity, and carbohydrate patterns. Morning insulin resistance, shift work, or steroid use may push the split toward more mealtime or basal coverage. Track patterns over several days before drawing conclusions.
Some clinicians discuss typical ranges such as 50/50 or 60/40, adjusted for meals, exercise, and hypoglycemia risk. If you use charts, consider context like meal size and timing. For a concise overview of visual frameworks, see Insulin Dosage Chart for a quick reference on structured dose planning. For consensus-based recommendations on insulin use and safety, consult the ADA Standards of Care in current-year updates.
Calculation Methods and Safety
People use several approaches to align doses with food and activity. An insulin dose calculation method typically combines carbohydrate counting, an insulin-to-carb ratio, and a correction factor for high readings. These frameworks help estimate meal coverage and correction doses. However, illness, stress, and timing can change needs quickly. Start conservatively, monitor closely, and check in with your care team before significant changes.
It helps to understand timing differences between rapid-acting insulin and regular human insulin. Onset and peak affect when you dose relative to meals. For a rundown of typical onset and peak windows, see the Rapid-Acting Insulin Guide to compare fast insulins and brand examples. To match mealtime insulin to your eating style, also review Prandial Insulin Types for timing and practical considerations.
Weight-Based Starting Points
Weight is sometimes used to estimate an initial daily insulin need before fine-tuning. In research and practice, clinicians may reference insulin dose per kg as a cautious starting framework, then individualize using glucose data. These figures are not prescriptions. They are orientation points that require adjustments for age, kidney function, and hypoglycemia history. Use them to understand the logic behind titration conversations.
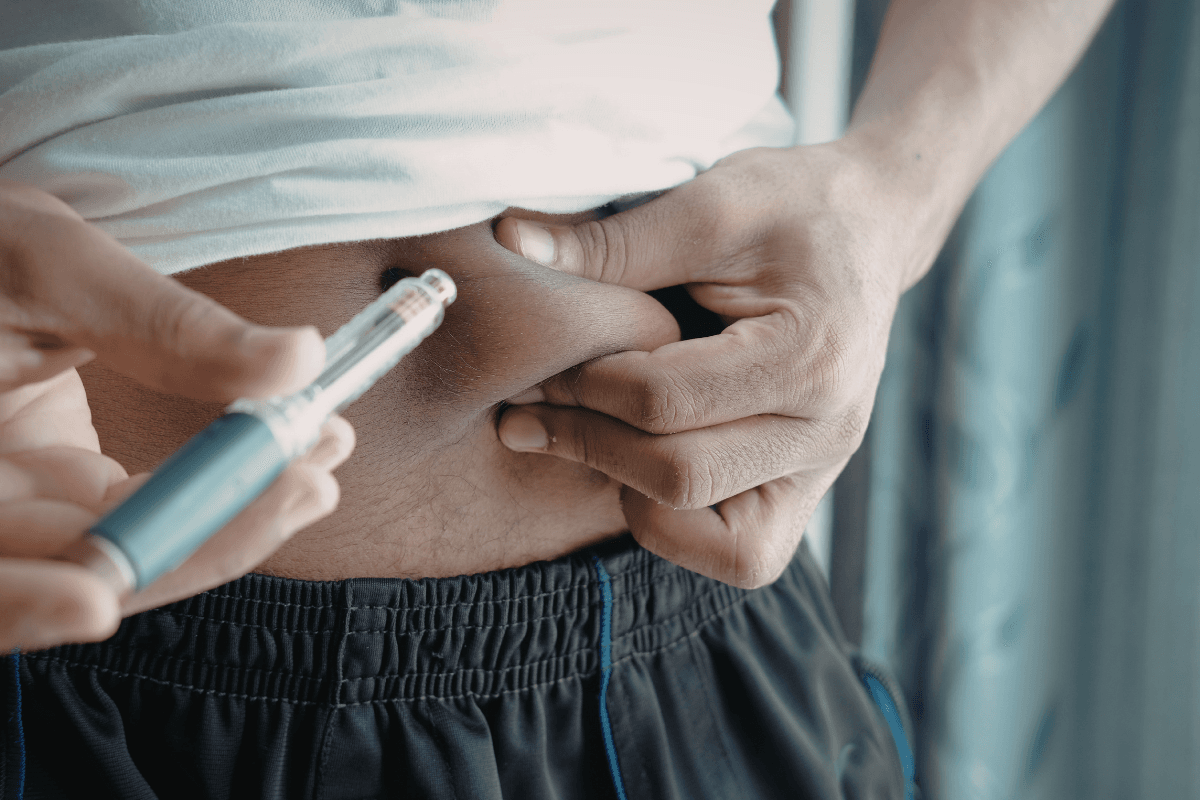
Injection route and technique also influence absorption and variability. Site rotation, needle length, and lipohypertrophy checks matter for consistent results. If you are reviewing delivery methods, see Ways of Administering Insulin for comparisons across pens, vials, and pumps, with practical trade-offs discussed inline.
Basal and Bolus Types with Examples
Knowing product families helps align action profiles with daily routines. Long-acting basal insulin examples include insulin glargine (Lantus, Basaglar, Toujeo), insulin detemir (Levemir), and insulin degludec (Tresiba). Intermediate-acting insulin includes NPH options such as Humulin N and Novolin ge NPH. These differ in duration and variability, which affects dosing frequency. Manufacturer labeling provides key pharmacokinetic details and safety considerations; see the Lantus prescribing information for an example of long-acting characteristics.
Bolus insulin includes rapid-acting analogs such as insulin lispro (Humalog), insulin aspart (NovoRapid), and insulin glulisine (Apidra), as well as regular human insulin (Humulin R, Novolin R). Action time and predictability vary across products and brands. If you are comparing specific long-acting choices, see Lantus vs Levemir for distinctions in duration and use-cases. For rapid-acting options used at meals, review Humulin vs Humalog for brand contrasts and timing notes.
Adjustments, Testing, and Troubleshooting
When fasting readings trend high or low, a structured basal insulin test may help reveal whether background coverage fits your needs. This method observes glucose during periods without food or bolus insulin to minimize confounders. People often repeat this on different days to confirm patterns before any change. Keep rescue carbs available and avoid testing if you are ill or unusually active.
Post-meal spikes may relate to carbohydrate estimates, timing, or insulin onset. Busy schedules can shift bolus timing and create mismatches. Reviewing fast-insulin timing can help; for a comparison of onset and peak ranges, see the Rapid-Acting Insulin Guide to understand how different brands behave around meals. Note: Any adjustments should be gradual and guided by your clinician to reduce hypoglycemia risk.
Practical Tools and Charts
Digital aids and tables can help visualize dosing logic. An insulin dose calculator by weight offers orientation for initial frameworks, but it cannot account for individual sensitivity, meal timing, or comorbidities. Use calculators as educational tools, not as stand-alone instructions. Cross-check with logs and professional guidance before adopting any changes.
Product characteristics also influence dose timing and variability. Understanding analog versus human insulin can clarify why two products behave differently at similar units. For a concise overview of structural differences, see Insulin Analogs to learn how molecular tweaks change action profiles. If you are considering non-basal-bolus options, preview Premixed Insulin for how fixed-ratio mixes alter flexibility and meal planning.
Regimens and Alternatives
Daily schedules, meal patterns, and coexisting conditions shape insulin plans. Examples of basal-bolus regimen structures include once-daily long-acting with bolus at each main meal, or twice-daily intermediate with rapid at meals. Some people use correction-only strategies during illness or travel, then revert to usual patterns once stable. Pumps and smart pens add other delivery options with different tracking features.
Fixed-ratio premixes may simplify dosing for some but reduce flexibility for snacking or varied meals. People comparing mix-based approaches often look at 70/30 or similar blends and how they fit their day. For background on fixed mixes and dose timing, see Premixed Insulin to understand trade-offs. If you are mapping comprehensive therapy structures in type 1 diabetes, Basal-Bolus Insulin Therapy offers a broader framework for regimen building and adjustment checkpoints.
Weight-Based Calculators and Visual Aids
Some educational resources use an insulin dose calculator by weight to sketch out totals before personalization. This can help learners see how daily dose estimates divide between background and meals, particularly early in therapy education. Keep in mind, calculators vary in assumptions, and results may not reflect your sensitivity, activity, or diet. Always interpret outputs as starting points for discussion, not action plans.
Visual tools such as charts and time-action curves can make differences between long-acting, intermediate, and rapid formulations clearer. Pair these with logs to spot trends across days rather than single readings. For further practical reading on matching insulin to real-life eating, review Prandial Insulin Types for timing nuances and dosing context that affect mealtime coverage.
Recap
Basal insulin steadies glucose between meals; bolus insulin targets meals and corrections. Ratios and weight-based frameworks are guides that require validation with your own data. Focus on patterns, timing, and product properties. Use structured tests, cautious adjustments, and professional input to align therapy with your lifestyle.
This content is for informational purposes only and is not a substitute for professional medical advice.