Please note: a valid prescription is required for all prescription medication.
Humira Product Overview: Uses, Safety, and Handling
Start 2026 with savings: Use code SAVE10 for 10% OFF all RX meds. Jan–1 Mar. Ozempic from Canada and Mounjaro Vial not included. Offer valid until March 1st. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
Price range: $1,131.99 through $2,242.99
You save


This page describes a prescription biologic medicine used for several inflammatory conditions. Humira is an adalimumab (a TNF blocker) treatment that is given by injection. It summarizes indications, dosing basics, safety topics, storage, and practical handling details to support informed discussions with a clinician.
What Humira Is and How It Works
Adalimumab is a monoclonal antibody (a targeted protein medicine) that reduces inflammation by blocking tumor necrosis factor (TNF), an immune-system signaling protein involved in inflammatory pathways. By lowering TNF activity, the treatment can reduce symptoms and help control disease activity in certain autoimmune conditions. This medicine is typically used long term and requires ongoing monitoring for infection and other risks.
Some patients explore Ships from Canada to US options when cross-border fulfilment is permitted. CanadianInsulin.com functions as a prescription referral platform and may confirm prescription details with the prescriber. When permitted, dispensing and fulfilment are completed by licensed third-party pharmacies.
The product is supplied in injection devices designed for at-home use after training. It is not a steroid, and it works differently than common anti-inflammatory drugs such as NSAIDs (nonsteroidal anti-inflammatory drugs). Because it affects immune function, clinical teams often review vaccination status, infection history, and certain baseline tests before starting therapy.
Who It’s For
This medicine is prescribed for selected inflammatory diseases where TNF plays a key role. Indications can include rheumatologic conditions such as rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, as well as gastrointestinal conditions like Crohn’s disease and ulcerative colitis. It may also be used in other immune-mediated disorders depending on local approvals and the prescriber’s judgment.
It is not appropriate for everyone. People with active serious infections (such as untreated tuberculosis) generally should not start a TNF blocker until evaluation and treatment are addressed. A clinician may also weigh risks differently in patients with recurrent infections, certain neurologic conditions (for example, demyelinating disorders), moderate-to-severe heart failure, or a history of some cancers. Gastrointestinal Category can be a helpful hub for broader digestive-health context, especially for patients navigating inflammatory bowel disease information.
Dosage and Usage
Dosing schedules vary by condition, age group, and prior treatment history. Some diagnoses use an initial “loading” phase followed by a maintenance schedule, while others start directly on maintenance. A clinician will select the regimen and may adjust timing based on response, tolerability, and other medicines used alongside it (such as methotrexate for certain arthritis indications). Do not change the dose or schedule without prescriber guidance.
Quick tip: If you are learning self-injection, ask for a step-by-step demo and written instructions.
Injection technique overview
The medicine is injected subcutaneously (under the skin), commonly in the abdomen or thigh, avoiding areas that are tender, bruised, scarred, or affected by psoriasis plaques. Rotate injection sites to reduce local irritation. Many patients use a prefilled pen or syringe and receive training on preparation, needle safety, and disposal in a sharps container. Before injecting, visually inspect the solution for particles or discoloration as directed by the labeling, and allow it to reach room temperature if the instructions recommend doing so. If an injection is painful or a strong skin reaction occurs, document what happened and discuss it with the care team.
Strengths and Forms
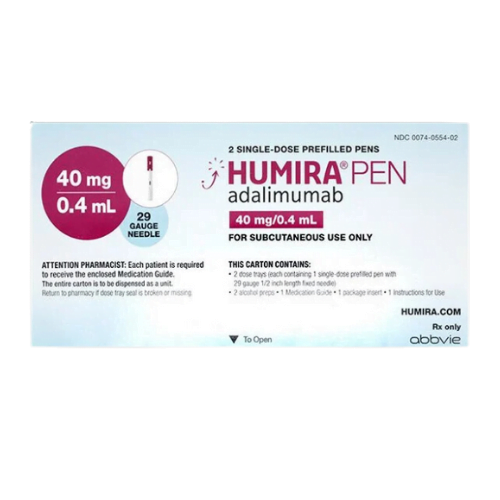
This medicine is available in several presentations that may include a prefilled syringe and an auto-injector style pen. Common strengths in circulation include 40 mg pens (with different fill volumes such as 0.8 mL or 0.4 mL depending on the specific presentation) and 80 mg/0.8 mL formats. Packaging, needle covers, and device steps can differ between versions, so device training should match the specific box you receive.
Availability can vary by jurisdiction, supplier, and formulary rules. If a prescriber writes for a specific device type (for example, a pen versus a syringe), it helps to confirm that the dispensed form matches the prescription. For patients with dexterity challenges, pen devices may be preferred, while others may choose a syringe for more control under clinician guidance.
Storage and Travel Basics
As a temperature-sensitive biologic, this medicine is usually stored refrigerated and protected from light. Do not freeze it, and do not use it if it has been frozen. Many versions can be kept at room temperature for a limited period, but the allowed time and the maximum room temperature can differ by presentation. Always confirm the specific storage instructions printed on the carton and patient leaflet for your product.
For travel, plan for temperature control and safe transport of injection supplies. Keep the device in its original packaging until use to help protect it from light, and bring a sharps container option for proper disposal. If you are crossing time zones, discuss timing considerations with the prescriber rather than independently shifting the schedule.
Why it matters: Heat or freezing can damage biologics and reduce reliability.
Side Effects and Safety
Like other TNF blockers, this treatment can increase the risk of infections because it dampens parts of the immune response. Commonly reported side effects may include injection-site reactions (redness, pain, itching), headache, rash, and upper respiratory symptoms. Patients are often advised to report fever, persistent cough, shortness of breath, painful urination, or other signs of infection promptly, because infections can become serious more quickly on immune-modifying therapy.
Serious risks can include tuberculosis or other opportunistic infections, hepatitis B reactivation in carriers, blood abnormalities, and rare immune-mediated or neurologic reactions. Some people may need screening tests before starting and periodic monitoring after initiation. If you also manage diabetes or circulation issues, keeping skin and foot health in mind is important; resources such as Diabetic Foot Ulcer and Diabetes Swollen Feet Symptoms can support general self-care discussions. For a practical framework on tracking adverse effects across medicines, see Side Effects Can Expect.
Drug Interactions and Cautions
This medicine is often used with other therapies, but combinations should be clinician-directed. Using more than one biologic immune suppressant at the same time can increase infection risk and is typically avoided unless a specialist has a clear rationale. Tell the care team about all prescription drugs, over-the-counter products, and supplements, including intermittent steroid courses and any recent antibiotics.
Vaccines require planning. Live vaccines are generally avoided during treatment with TNF blockers, and clinicians may recommend certain immunizations before starting therapy. If surgery or dental procedures are planned, the prescriber may give timing instructions to reduce infection risk while balancing disease control. If you have a history of fractures or bone fragility from long-term inflammation or steroid exposure, background reading like Fragile Connection Bone Fractures may be useful for broader context to discuss with your clinicians.
Compare With Alternatives
Several other biologics and advanced therapies may be used for similar conditions, and the right choice depends on the diagnosis, prior response, and safety considerations. Alternatives may include other TNF inhibitors (such as etanercept or infliximab) or non-TNF biologics (for example, agents that target different immune pathways in inflammatory bowel disease or psoriasis). In some settings, adalimumab biosimilars may also be available, and a clinician can explain whether switching is appropriate and how product substitution rules work locally.
Device style, dosing frequency, monitoring needs, and formulary requirements can differ between options. Browsing hubs like Gastrointestinal Products may help patients understand what types of therapies exist across GI conditions, without implying any specific choice. Separately, some people using immune therapies also manage unrelated chronic diseases; examples of non-equivalent medicines on the site include Tradjenta and Onglyza, which are for type 2 diabetes and are not substitutes for a TNF blocker.
Pricing and Access
Out-of-pocket cost for Humira can vary widely based on insurance design, formulary tiering, prior authorization requirements, and whether the prescription is routed through a specialty pharmacy network. Coverage rules may also differ between private plans and public programs, including Medicare, and some plans are administered through pharmacy benefit managers such as CVS Caremark, Express Scripts, or OptumRx. In addition to coverage variation, clinical documentation (for example, diagnosis and past therapies) may be needed to support approval.
Some patients pursue cash-pay approaches or seek options without insurance, depending on eligibility and jurisdictional rules. As a referral platform, CanadianInsulin.com may need to verify prescription details with the prescriber before coordination, and fulfilment is handled by licensed pharmacies where permitted. For general context on available site-wide information, Promotions may list ongoing programs or updates, but specific coverage decisions remain with the insurer and prescriber.
Authoritative Sources
For the most reliable prescribing details, consult official labeling and reputable clinical references. A neutral starting point is the U.S. National Library of Medicine’s labeling database: DailyMed drug labeling.
For regulatory safety communications and product class information, review: FDA Drugs.
For patient-friendly background on inflammatory bowel disease care, see: Crohn’s & Colitis Foundation.
When temperature-controlled transport is used, prompt, express, cold-chain shipping may help protect refrigerated medicines during transit.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
Is Humira the same as adalimumab?
Adalimumab is the generic (nonproprietary) drug name; Humira is a brand-name version of adalimumab. In many places, other adalimumab products (including biosimilars) may also be available. While they target the same immune pathway (TNF), products can differ in device design, allowed indications, and substitution rules depending on local regulations. A clinician and pharmacist can confirm whether a specific prescribed product can be interchanged and what to expect if the presentation changes.
What conditions is Humira commonly prescribed for?
Humira is prescribed for several immune-mediated inflammatory conditions. These can include rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis. It may also be used for other approved indications depending on the country and local labeling. Because each condition has different treatment goals and monitoring needs, the prescribing specialist typically selects the regimen based on diagnosis, prior therapies, and individual risk factors.
What screening or monitoring is needed before and during treatment?
Clinicians often screen for infections that can worsen on immune-modifying therapy, such as tuberculosis, and may review hepatitis status when relevant. Baseline and follow-up monitoring can also include symptom checks for infection, review of vaccination status, and periodic labs when clinically indicated. The exact plan depends on the underlying condition, other medicines, and medical history. Contact the care team promptly for fever, persistent cough, shortness of breath, or other concerning infection symptoms.
Can I get vaccines while using Humira?
Vaccination plans should be discussed with the prescribing clinician. Many inactivated (non-live) vaccines may still be given, but timing can matter. Live vaccines are often avoided during treatment with TNF blockers due to infection risk. If travel vaccines are needed, or if routine immunizations are due, clinicians may recommend completing certain vaccines before starting therapy. Always tell the care team about upcoming vaccines, recent exposures, and any history of recurrent infections.
How should I store a Humira pen at home or while traveling?
This medicine is generally stored refrigerated and protected from light, and it should not be frozen. Some versions may allow limited room-temperature storage, but the permitted duration and conditions depend on the specific presentation and labeling. For travel, keep the device in its original carton, plan for temperature control, and bring supplies for safe sharps disposal. If you suspect the product was exposed to freezing or excessive heat, consult a pharmacist for next steps rather than using it.
What should I ask my clinician before starting Humira?
Useful topics include: your infection history (including past tuberculosis exposure), current vaccines, and whether any screening tests are needed first. Ask how to recognize infection warning signs and when to seek urgent care. It also helps to review your full medication list, including steroids, other biologics, and supplements, because combinations can raise risk. If you are pregnant, planning pregnancy, or breastfeeding, discuss how risks and benefits are weighed for your situation.
What happens if I miss a dose?
If a dose is missed, the safest approach is to follow the instructions provided with the product and the plan set by the prescriber. Do not double up doses unless a clinician specifically directs it. If you are unsure when the next injection should be taken, contact the prescribing clinic or pharmacist with the date of the last dose and your usual schedule. Keeping a written dosing calendar or reminder can reduce missed doses over time.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
DPP-4 Inhibitors Weight Loss: What Research Shows Clinically
Key Takeaways DPP-4 inhibitors usually have little effect on body weight. Most studies describe this class as “weight neutral,” not weight-loss therapy. Weight change often depends more on diet, activity,…
Sitagliptin Side Effects: Practical Signs, Risks, Next Steps
Key Takeaways Most reactions are mild, but pattern matters. Stomach upset and diarrhea can occur, especially with metformin. Rash and swelling need prompt evaluation for allergy. Severe abdominal pain is…
Best GLP-1 Supplement for Weight Loss: Evidence and Safety
GLP-1 is a gut hormone tied to appetite and blood sugar control. Prescription GLP-1 drugs act directly on GLP-1 receptors. Supplements do not. That difference is why many “GLP-1” products…
Contour Next Test Strips Practical Use And Compatibility Checks
Key Takeaways Contour Next Test Strips are single-use, in vitro diagnostic strips used with compatible glucose meters. Small details on the box and your technique can affect results. Match strip…