Families and clinicians continue seeking disease-modifying options for early Alzheimer’s disease. This guide summarizes benefits, risks, dosing logistics, trial findings, and regulatory context to help informed discussions.
Key Takeaways
- Early-stage focus: Intended for mild cognitive impairment and mild dementia.
- Targeted action: Designed to clear amyloid beta plaques in the brain.
- Monitoring matters: MRI screening helps identify ARIA changes early.
- Balanced decisions: Benefits must be weighed against infusion risks.
Leqembi may help reduce amyloid burden in appropriately selected patients. Understanding how this therapy is given and monitored supports safer, more confident choices.
Benefits and Indications
This monoclonal antibody targets amyloid beta (a protein fragment) linked to Alzheimer’s pathology. In clinical studies, treatment was associated with less amyloid on brain imaging and slower decline on certain cognitive and functional scales. These outcomes may translate into modest, clinically meaningful differences for some people in the early disease stages. The indication focuses on mild cognitive impairment due to Alzheimer’s and mild dementia, reflecting where benefit–risk balance appears most favorable today.
Many caregivers ask “Who makes Leqembi” before discussing support services. The therapy is developed by Eisai, with Biogen as a commercial partner. Ask about educational resources and any patient support offered by the manufacturer, as coordination can ease MRI scheduling and infusion logistics. For broader disease context and caregiver resources, see World Alzheimer’s Day for community awareness and support materials.
How Leqembi Works (Mechanism and Targets)
The drug binds aggregated forms of amyloid beta to promote plaque clearance. This process reflects its pharmacologic mechanism, often described as disease-modifying rather than symptomatic. Research suggests the greatest impact occurs earlier, when amyloid burden remains substantial and neuronal networks retain more function. This timing aligns with diagnostic pathways emphasizing early recognition and biomarker confirmation where available.
Clinicians may describe this as the Leqembi mechanism of action, contrasting with symptomatic agents like cholinesterase inhibitors (memory-boosters). Donanemab and similar antibodies also target amyloid, though epitope preferences differ. While precise biological pathways are complex, the practical takeaway is consistent: plaque reduction can track with slower decline for some patients, but outcomes vary. For current treatment developments beyond antibodies, see Semaglutide Alzheimer Phase 3 Trials for ongoing research in metabolic pathways.
Infusion and Monitoring
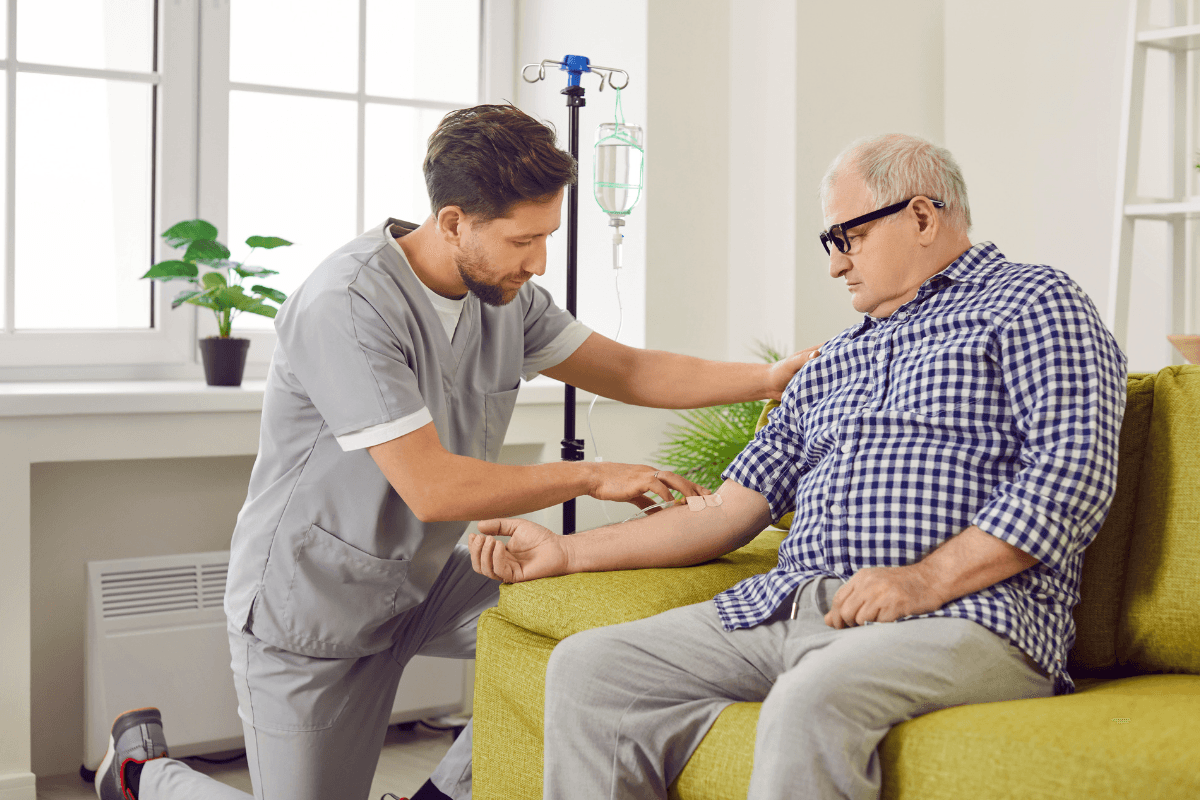
Therapy is administered by intravenous infusion (IV; medicine delivered into a vein). A typical visit includes a brief clinical check, the infusion itself, and post-infusion observation. Centers screen for infusion reactions, such as headache or nausea, and provide supportive care if needed. Facility experience and clear protocols help reduce delays and missed monitoring steps.
Your care team will outline the Leqembi infusion protocol, including pre-treatment MRI assessments to screen for ARIA (amyloid-related imaging abnormalities). Follow-up MRIs at defined intervals help identify changes early, especially in the first treatment months. For practical scheduling and dose-interval details, see Leqembi Dosing for step-by-step administration guidance and planning considerations.
Safety and Side Effects
Clinicians watch for ARIA, a spectrum of MRI-detected brain changes that can include vasogenic edema (fluid shifts) or microhemorrhages (tiny bleeds). Symptoms vary and may include headache, confusion, dizziness, or visual changes. Most events are mild to moderate, but serious outcomes can occur, so vigilance and timely imaging matter. The risk may be higher in certain genetic backgrounds, such as APOE ε4 carriers, reinforcing the role of shared decision-making.
Discuss potential risks as “Leqembi side effects” in routine visits, with clear instructions for reporting new neurologic symptoms. Clinics often provide after-hours guidance for sudden changes. For a deeper look at symptom patterns and mitigation strategies, see Exploring Leqembi Side Effects for structured risk overviews and monitoring tips. Comorbid conditions can complicate cognition; for overlapping concerns, see Diabetes and Dementia for context on metabolic health and cognitive decline.
Approvals and Access
Regulators in the United States granted an initial accelerated approval followed by a traditional approval based on confirmatory data. This pathway underscores the balance between addressing urgent needs and verifying clinical benefit. Payers may require documentation of diagnosis, disease stage, and imaging before coverage approval. Health systems often establish eligibility criteria and observation protocols to standardize safe use.
When discussing coverage, clinicians sometimes reference Leqembi FDA approval to align documentation with payer criteria. For a neutral regulatory summary, review the U.S. Food and Drug Administration’s FDA approval announcement, which outlines indications, trial support, and required safety monitoring. Regional policies vary, so confirm local requirements, documentation specifics, and care-site capabilities before scheduling infusion starts.
Comparing Antibodies: Donanemab and Kisunla
The field now includes multiple amyloid-targeting antibodies. Teams compare dosing schedules, monitoring intensity, and trial populations when selecting a therapy. Head-to-head data remain limited, so decisions rely on indirect comparisons and patient-specific risks. Practical factors, such as MRI access and infusion center location, also influence choice.
Clinicians may outline Leqembi vs Donanemab when discussing timing, imaging cadence, and eligible populations. For the latest regulatory context about donanemab, see the U.S. FDA’s FDA approves donanemab notice, which summarizes labeling and safety statements. For additional safety context on Eli Lilly’s product, see Kisunla Side Effects for ARIA patterns and practical monitoring advice. Broader therapy landscape articles, such as Can Ozempic Help With Alzheimer’s, can help frame ongoing research beyond antibodies.
Costs and Coverage Considerations
Affordability and access can be challenging with new biologics. Discuss insurance benefits, deductibles, and co-pay caps; ask about diagnostic coverage for MRIs and amyloid testing. Health systems may offer financial counseling to map likely out-of-pocket ranges. Manufacturer support programs sometimes provide educational or logistical assistance.
Conversations often center on Leqembi cost, but total care costs include imaging, infusion services, and monitoring visits. Request a written estimate that includes facility fees and follow-up scans. For breakdowns of components and planning considerations, see How Much Does Leqembi Cost to understand line items and potential cost offsets. Awareness initiatives like Brain Awareness Month 2025 can also point to nonprofit support resources.
Clinical Evidence Summary
Confirmatory studies evaluated cognition, function, and biomarker changes, including amyloid PET and plasma/CSF measures. Outcomes showed reduced amyloid burden and slower decline on select scales for many participants, though individual responses varied. Safety signals concentrated in early months, highlighting the importance of protocolized MRI monitoring. Efficacy depended on baseline characteristics, emphasizing careful diagnosis and staging before initiation.
Trial designs, eligibility criteria, and endpoints shape how results translate to practice. When reviewing data, focus on the primary endpoints and adverse event tables from pivotal studies. Clinicians may reference Leqembi clinical trial publications during shared decision-making to align expectations. For ongoing updates and related neurology topics, explore the Neurology category for curated, condition-focused resources.
Recap
This therapy aims to reduce amyloid burden and slow clinical decline in early Alzheimer’s. Risks require MRI surveillance, clear infusion protocols, and close symptom reporting. Coverage depends on documentation, stage eligibility, and local program capacity. For adjacent neurological content, see the Neurology Category for product context relevant to nervous system care.
Note: Decisions should reflect personal goals, support systems, and comorbidities. Structured follow-up improves safety and helps maintain continuity between clinic, imaging, and infusion services.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.