Understanding what does insulin do in the body helps you manage glucose safely. Insulin signals cells to use and store energy, while glucagon raises glucose when levels fall. Together, they keep blood sugar within a narrow, healthy range. This overview explains core biology and practical steps.
This guide suits people with diabetes, caregivers, and students. You will learn mechanisms in clear language, then see real-world tips on timing, monitoring, and storage. Where appropriate, we reference authoritative clinical sources.
Key Takeaways
- Core role: Insulin moves glucose into muscle and fat cells.
- Counterbalance: Glucagon raises glucose between meals and overnight.
- Resistance: Cells respond poorly, so insulin signals are blunted.
- Practice: Time basal and mealtime doses to food and activity.
- Safety: Store insulin correctly and prepare for hypoglycemia.
What Does Insulin Do in the Body
Insulin acts as a master metabolic signal. In muscle and fat cells, it increases glucose transporters on the cell surface, so sugar moves from blood into tissues. In the liver, it promotes glycogen synthesis (glucose storage) and curbs gluconeogenesis (new glucose production). This combination helps stabilize blood glucose after meals.
Insulin also influences fat and protein balance. It supports lipogenesis (fat building) and limits lipolysis (fat breakdown) when energy is plentiful. It supports protein synthesis in muscle and reduces protein breakdown during feeding. The net effect is energy storage when calories are available and preservation of lean tissue.
Insulin Basics: Structure, Source, and Storage
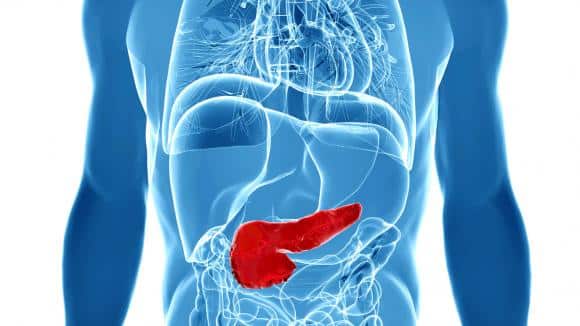
Clinically, insulin is a peptide hormone (a small protein) made as proinsulin, then split into active insulin and C‑peptide. In the pancreas, beta cells package insulin into granules and release it as blood glucose rises. Understanding this normal cycle makes treatment logic clearer.
If you have wondered where is insulin produced, it is synthesized in the pancreatic islets by beta cells. After release, insulin circulates, binds receptors, and is cleared mainly by the liver and kidneys. In the body, stored hormone sits inside beta‑cell granules until a glucose surge triggers exocytosis. Replacement insulin for therapy is manufactured to mimic these patterns.
Artificial Production and Types
Modern human insulin and analogs are made by recombinant DNA methods in cultured yeast or bacteria. Engineers adjust amino acids to change onset and duration. Rapid-acting analogs are designed for meals, while basal analogs provide steady, daylong coverage. For examples of rapid options used at mealtimes, see NovoRapid Vials for product characteristics and timing context. For a common basal option that provides background coverage, see Lantus Cartridges as a reference formulation.
How Insulin Works: Glucose Uptake and Metabolism
At the cell surface, insulin binds its receptor and triggers signaling cascades. One key result is moving GLUT4 transporters to the membrane in muscle and fat cells. This step increases glucose entry, supports glycogen formation, and supplies energy for activity.
Clinically, people ask how does insulin work. In short, it lowers circulating glucose by promoting uptake and by inhibiting hepatic glucose output. For a concise overview of hormone control of glucose, the NIDDK overview of diabetes summarizes insulin’s role and liver regulation. For context on therapies that complement insulin action, see Common Diabetes Medications for mechanisms beyond insulin alone.
Glucagon and Counter-Regulation
People often ask what is glucagon because it acts opposite to insulin. Glucagon is a peptide hormone from pancreatic alpha cells that raises blood glucose during fasting. It stimulates glycogenolysis (glycogen breakdown) and gluconeogenesis in the liver, keeping the brain supplied with fuel overnight and between meals.
Insulin and glucagon form a paired system. After eating, insulin predominates and drives storage. During fasting, glucagon predominates and mobilizes fuel. For background on autoimmune beta‑cell loss and its impact on this balance, see Type 1 Diabetes for context on insufficient endogenous insulin.
Glucagon Use and Emergencies
In severe hypoglycemia, every minute matters. Families and caregivers should know how does glucagon work and when to use an emergency kit. Glucagon triggers the liver to release glucose quickly, especially when oral carbohydrates are not possible due to confusion or unconsciousness.
Emergency products and training vary by device. For regulatory details on indications and administration, review the FDA-approved glucagon label to understand safety warnings and use scenarios. For broader supplies you may need for diabetes care planning, see our Diabetes Products section for device options discussed in educational resources.
Note: Teach household members where the kit is stored and practice the steps with trainer devices when available.
Insulin Resistance and Type 2 Care
Clinically, what is insulin resistance means cells respond weakly to normal insulin levels. The pancreas compensates by secreting more hormone, but over time glucose rises. Contributors include genetics, excess visceral fat, physical inactivity, certain medicines, and sleep disruption.
Management focuses on nutrition, physical activity, weight reduction, and medications that improve sensitivity or support insulin. For an example of basal insulin combined with a GLP‑1 therapy, see Xultophy Prefilled Pen for clinical background on combination approaches. For cardiometabolic context on incretin-based therapies, see Mounjaro Heart Benefits for evidence summaries beyond glucose control.
Practical Use: Timing and Monitoring
Your plan should align insulin type, meals, and activity. Providers often individualize basal dosing to cover 24 hours and bolus dosing for carbohydrates. Guidance on when to take insulin for type 2 diabetes depends on insulin type, meal timing, and your glucose patterns.
Monitoring helps you learn patterns and reduce lows. Many people check glucose before meals, sometimes two hours after, and at bedtime to see post‑meal changes. If you use mealtime insulin, work with your care team to decide when to check your glucose after a dose to assess coverage. For background on device choices and injection techniques, browse our Type 2 Diabetes library for technique guides and education pieces. For background on brand options and biosimilars, see Basaglar Generic Name to understand therapeutic alternatives.
Safety, Storage, and Stability
Insulin potency depends on temperature and time. Unopened vials and pens usually stay refrigerated; opened products often can remain at room temperature for a limited time. Do not freeze insulin, avoid direct heat and sunlight, and discard it if it looks cloudy or forms clumps when it should be clear.
Always confirm the storage instructions for your specific brand. For general principles of insulin handling and syringe safety, the American Diabetes Association has practical guidance; see their insulin storage and syringe safety overview for temperature ranges and expiration basics. For medication comparisons that may affect storage needs, see Common Diabetes Medications to understand formulation differences.
Recap
Insulin enables cells to use and store glucose, while glucagon helps release it during fasting. Resistance blunts these signals, raising blood sugar over time. Pair sound biology with practical timing, monitoring, and storage to keep daily care safer and steadier.
Further reading across our site includes therapy overviews and device education. Explore Diabetes Articles for structured guides and updates throughout the year.
This content is for informational purposes only and is not a substitute for professional medical advice.