Please note: a valid prescription is required for all prescription medication.
Ozempic Uses and Safety Overview
Recent price drop plus an extra $50 off when you order 2 or more Ozempic products from Canada - Use Code: OZEMPIC50. For International Ozempic products, use coupon SAVE10 and get a 10% discount. Offer valid until March 1st. Coupon code cannot be combined with other offers. Maximum allowable quantity equal to a 90 day supply per single order.
Price range: $249.99 through $299.99
You save


Ozempic is a prescription, once-weekly injectable medicine that contains semaglutide, a GLP-1 receptor agonist used in adults with type 2 diabetes to help improve blood glucose control, and in some settings it is also used to reduce certain cardiovascular risks. It is not insulin, and it works by supporting glucose-dependent insulin release, lowering glucagon (a hormone that raises glucose), and slowing stomach emptying, which can also affect appetite. Some patients explore Ships from Canada to US as part of planning for ongoing therapy, and this page summarizes key label-aligned points on dosing basics, safety, storage, and practical access topics for informed discussions with a clinician.
What Ozempic Is and How It Works
Semaglutide belongs to the GLP-1 receptor agonist class, a group of medicines used for type 2 diabetes that mimic the activity of a natural gut hormone released after eating. In plain terms, this class helps the body respond to meals more effectively by increasing insulin release only when glucose is elevated and by reducing glucagon signals from the liver. It can also slow gastric emptying, which may increase feelings of fullness and reduce post-meal glucose spikes. If you are reviewing diagnosis context or treatment categories, the Type 2 Diabetes hub and the GLP 1 Agonists collection can help you compare related options at a high level.
Because this treatment is prescription-only, CanadianInsulin can help confirm prescription details with your prescriber before referral. Mechanistically, GLP-1 medicines are often described as “glucose-dependent,” which is one reason they are used alongside lifestyle measures and, when appropriate, other diabetes therapies. Effects on appetite and body weight can occur, but the intended clinical goal on the diabetes label is improved glycemic control and risk management, not rapid weight reduction. Response and tolerability vary, and the prescriber’s plan usually includes a gradual dose-escalation schedule to reduce gastrointestinal side effects.
Who It’s For
Ozempic is generally prescribed for adults with type 2 diabetes as part of an overall plan that includes nutrition, activity, and monitoring. It may be considered when A1C goals are not met with other medicines, when weight change is a relevant factor, or when clinicians prioritize therapies with cardiovascular benefit depending on the individual’s history and local labeling. Some people also ask about using semaglutide for obesity management; that can involve off-label decision-making and should be approached carefully, especially when appetite suppression may complicate disordered eating patterns. For broader context on weight-related indications and non-medication supports, the Obesity Hub and Weight Management Articles hub may be useful starting points.
This medicine is not used for type 1 diabetes or diabetic ketoacidosis (DKA). It is also not appropriate for everyone due to contraindications and boxed warnings on the label, including a history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2). Clinicians may use added caution in people with prior pancreatitis, significant gastrointestinal disease (such as severe gastroparesis), gallbladder disease, or advanced kidney problems, especially if dehydration could worsen renal function. Pregnancy and breastfeeding considerations should be discussed with a clinician, since plans may need to change before conception or during pregnancy.
Dosage and Usage
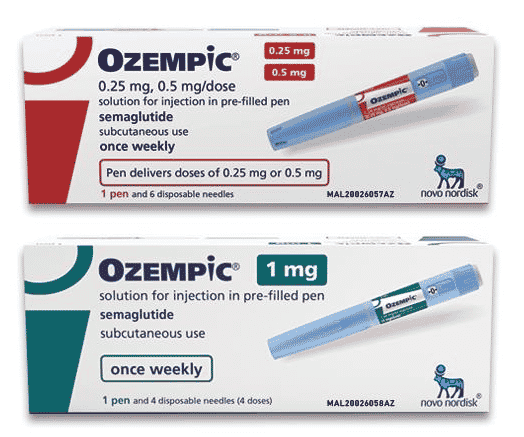
Ozempic is injected once weekly on the same day each week, with dose increases typically made in steps to improve tolerability. Many protocols begin with a low starter dose and then increase after several weeks; common pen dose steps discussed in prescribing information include 0.25 mg, then 0.5 mg, and potentially 1 mg as directed by the prescriber. Exact schedules and maximum doses depend on the local product label, clinical goals, and how a person responds, so it is important to follow the prescriber’s written instructions and the package insert. For a label-focused walkthrough, see Dosage Guide Basics.
Why it matters: Gradual escalation can reduce nausea and other stomach-related side effects.
Administration is usually subcutaneous (under the skin) in the abdomen, thigh, or upper arm, with rotation of injection sites to reduce irritation. Pens and needles should not be shared, even if the needle is changed, due to infection risk. Training on pen technique and safe disposal of sharps is typically provided by a clinic or pharmacist. If a dose is missed, the product labeling gives timing rules for whether to take it soon or skip and resume the next scheduled dose; it is generally not recommended to “double up.” People who also use insulin or sulfonylureas may need a clinician-guided plan to reduce hypoglycemia risk while titrating.
Strengths and Forms
Ozempic is supplied as a prefilled, multi-dose pen for subcutaneous injection. Pens are designed to deliver set dose amounts, and packaging details (such as total volume, concentration, and the number of doses per pen) can differ by jurisdiction and presentation. It helps to confirm that the pen you have matches the prescribed dose step and that the dose selector functions as intended. Pharmacists may also provide a quick check on pen handling, including needle attachment and priming steps, based on the specific device.
The product is not a tablet, which matters for people searching for “semaglutide pill” or “oral semaglutide.” Oral semaglutide is a different formulation with different administration rules (including fasting requirements) and is not interchangeable on a milligram-to-milligram basis with injections. Availability of presentations can vary. The table below summarizes commonly referenced dose steps for the injectable pen; always confirm your exact pen label and instructions.
| Form | Route | Common dose steps | Notes |
|---|---|---|---|
| Prefilled pen | Subcutaneous | 0.25 mg, 0.5 mg, 1 mg | Escalation and maintenance depend on labeling and clinical plan |
Storage and Travel Basics
Unopened pens are typically stored in a refrigerator and protected from light, and they should not be frozen. Once in use, labeling commonly allows either refrigerated or room-temperature storage for a limited period; the exact in-use timeframe and temperature limits should be verified on the package insert that comes with the pen you have. If there is any concern that the medication was exposed to extreme heat, freezing temperatures, or prolonged light exposure, a pharmacist can help determine whether it should be replaced. If the solution appears cloudy, discolored, or contains particles, it should not be used.
Quick tip: Keep the pen in carry-on luggage and avoid direct contact with ice packs.
For travel planning, focus on temperature stability, safe needle disposal, and maintaining your weekly schedule across time zones. Many people use insulated bags and keep medicines away from car dashboards or checked luggage compartments that can overheat or freeze. It is also helpful to bring extra needles, alcohol swabs, and a copy of the prescription label. A practical checklist is available in Travel With Injections, which covers common real-world scenarios like airport screening and hotel refrigeration. If you use a continuous glucose monitor or test strips, pack them together so monitoring remains consistent while away from home.
Side Effects and Safety
The most common side effects of GLP-1 receptor agonists are gastrointestinal and often appear during dose escalation. Typical issues include nausea, vomiting, diarrhea, constipation, stomach discomfort, and decreased appetite. These effects can be mild or disruptive, and dehydration can become a concern if vomiting or diarrhea is persistent. Eating smaller meals, avoiding high-fat foods during titration, and keeping up with fluids may help some people, but persistent symptoms should be reviewed with a clinician. For a patient-focused overview of red flags and practical precautions, see Practical Safety Guide.
Serious risks discussed in labeling can include pancreatitis, gallbladder disease (such as gallstones), worsening kidney function from volume depletion, severe allergic reactions, and hypoglycemia when used with insulin or insulin secretagogues (for example, sulfonylureas). Ozempic also carries a boxed warning related to thyroid C-cell tumors seen in rodent studies; it is contraindicated in people with MTC or MEN 2 history. Some individuals with diabetes may have diabetic retinopathy (eye disease); rapid glucose improvement can sometimes coincide with worsening eye symptoms, so vision changes should prompt medical review. If severe abdominal pain, signs of dehydration, or allergic symptoms occur, urgent evaluation is appropriate.
Drug Interactions and Cautions
This class can slow gastric emptying, which may affect the absorption of some oral medicines. The effect is often modest, but it can matter for drugs that require precise timing or have a narrow therapeutic index (where small level changes can be significant). A clinician or pharmacist should review all prescription medicines, over-the-counter products, and supplements, including thyroid medications, anticoagulants, and any diabetes agents that raise hypoglycemia risk. Alcohol use can also complicate glucose patterns and dehydration risk, especially when appetite is reduced or nausea occurs.
It is usually not recommended to combine multiple GLP-1 receptor agonists at the same time. Caution is also warranted when people consider compounded versions of semaglutide or “semaglutide compound” products, because formulations, dosing accuracy, and oversight can differ from approved products. If switching between GLP-1 therapies or changing between injectable and oral formulations, prescribers typically use a structured plan rather than a direct swap. During changes, monitoring of glucose trends and side effects is often emphasized to reduce the risk of overtreatment, dehydration, or intolerable gastrointestinal symptoms.
Compare With Alternatives
People often compare Ozempic with other incretin-based options and weight-management medicines, but the “best” choice depends on the indication, prior therapy, side effect tolerance, and cardiovascular or kidney considerations. Another semaglutide product, Wegovy, is labeled for chronic weight management in specific populations and uses a different dosing regimen; for basic product information, see the Wegovy Product Page. If the goal is an oral formulation for type 2 diabetes, oral semaglutide (Rybelsus) may be discussed, with distinct administration rules; see the Rybelsus Semaglutide Pills listing for form details.
Another common comparison is with tirzepatide (a dual GIP/GLP-1 agonist), which is a different molecule and has its own labeling and titration approach. Differences between semaglutide and tirzepatide often relate to side effect patterns, dosing steps, and the approved indication rather than a simple “stronger vs weaker” framing. If you want a mechanism-focused overview written for patients, Tirzepatide Vs Semaglutide summarizes the main distinctions. People also ask about “generic” or “compound” versions; a pharmacist can help clarify what is approved and what is not interchangeable.
Pricing and Access
Coverage and access for GLP-1 medicines can vary widely by plan, diagnosis, and local policies, and documentation requirements may change over time. Dispensing is handled by licensed third-party pharmacies where permitted. Prescribers may be asked for details such as diagnosis codes, recent A1C values, prior medication trials, or clinical rationale when insurers apply prior authorization or step therapy rules. For some patients, the main barrier is formulary placement; for others, it is tolerance of titration or coordination with other diabetes medications.
For people paying cash or managing therapy without insurance, the out-of-pocket amount can depend on dose step, pen presentation, and pharmacy pricing policies, and it may change between refills. Planning tips for budgeting and paperwork are summarized in Out Of Pocket Planning. If you are reviewing general site-wide programs, the Promotions Page provides an overview of available options, when offered, without implying eligibility for any specific patient.
Cross-border fulfilment may be considered based on eligibility and jurisdiction. In all cases, the safest path is to keep the prescriber informed about the exact product, dose step, and device you are using, and to reconcile the medication list at each visit. If interruptions occur due to coverage changes or tolerability, clinicians may recommend a structured restart plan rather than resuming a higher dose immediately, because gastrointestinal side effects can recur after gaps.
Authoritative Sources
For the most current, jurisdiction-specific instructions, confirm details in the official prescribing information.
FDA prescribing information details and boxed warning: FDA Label for Ozempic semaglutide injection.
Drug safety and use instructions in a federal monograph format: DailyMed drug labeling database.
Clinical standards for diabetes care and medication selection: American Diabetes Association Standards of Care.
When temperature-sensitive medicines are packaged by the dispensing pharmacy, they may be prepared for prompt, express, cold-chain shipping when appropriate.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is Ozempic used for?
Ozempic is a prescription injectable medicine containing semaglutide. It is used in adults with type 2 diabetes to improve blood glucose control alongside diet and physical activity. Depending on the approved labeling in your location, it may also be indicated to reduce the risk of certain cardiovascular events in adults with type 2 diabetes and established cardiovascular disease. It is not used for type 1 diabetes or diabetic ketoacidosis. A clinician should review your history, current medicines, and goals before starting or changing therapy.
Is Ozempic approved for weight loss?
In many jurisdictions, Ozempic is approved for type 2 diabetes, not specifically for chronic weight management. Some clinicians may prescribe semaglutide products off-label for weight-related goals when they judge benefits outweigh risks, but that decision should account for contraindications, mental health history, and monitoring needs. A different semaglutide product may be labeled for chronic weight management with its own dose-escalation schedule. If weight change is a primary goal, ask a clinician which product is indicated and how follow-up will be handled.
What doses are commonly used with semaglutide pens?
Semaglutide injection pens are typically used with a stepwise titration plan to reduce side effects. Common dose steps discussed in prescribing information include 0.25 mg weekly as a starter dose, then 0.5 mg weekly, and potentially 1 mg weekly as directed. Not every person needs higher steps, and dose selection depends on glucose targets, tolerance, and local labeling. Do not adjust the dose based on symptoms alone. If there is a gap in therapy, a clinician may recommend restarting at a lower step.
What side effects should I watch for while taking Ozempic?
The most common side effects are gastrointestinal, including nausea, vomiting, diarrhea, constipation, abdominal discomfort, and reduced appetite, especially during dose increases. Contact a clinician if symptoms are severe or persistent, or if you cannot keep fluids down. Seek urgent care for severe abdominal pain that may suggest pancreatitis, signs of an allergic reaction, or symptoms of dehydration (dizziness, reduced urination). If you use insulin or a sulfonylurea, watch for hypoglycemia symptoms such as shaking, sweating, or confusion.
Can Ozempic be used with insulin or other diabetes medicines?
It may be used with other diabetes medicines, but combinations require planning. The risk of hypoglycemia is higher when semaglutide is used with insulin or insulin secretagogues (such as sulfonylureas), so prescribers sometimes adjust those agents when starting or titrating. Other combinations may raise tolerability issues, such as overlapping gastrointestinal side effects. Do not combine multiple GLP-1 receptor agonists unless a specialist specifically directs it. A complete medication review with a pharmacist or clinician helps avoid duplications and reduces safety risks.
How should I store semaglutide pens and handle travel?
Unopened pens are usually refrigerated and protected from light, and they should not be frozen. After first use, the label often allows either refrigerated or room-temperature storage for a limited period, but the exact timeframe and temperature limits can vary by product and jurisdiction. For travel, keep the pen in carry-on luggage, avoid leaving it in a hot car, and prevent direct contact with ice packs. Bring extra needles and a sharps plan. If exposure to extreme temperatures is suspected, ask a pharmacist whether replacement is needed.
What should I ask my clinician before starting semaglutide?
Ask how the medicine fits your overall diabetes plan, including targets for A1C, fasting glucose, and weight-related goals. Confirm contraindications and warnings, especially any personal or family history of medullary thyroid carcinoma or MEN 2, prior pancreatitis, gallbladder disease, or significant kidney problems. Review your full medication list for hypoglycemia risk and timing issues with oral drugs. Discuss what monitoring is expected (glucose logs, symptoms, eye exams if you have retinopathy) and what to do if doses are missed or side effects become limiting.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
SGLT2 Inhibitors Explained: Uses, Risks, and Examples
Key Takeaways These medicines lower blood sugar by acting in the kidneys. Some are also labeled for heart failure or chronic kidney disease. Drug names include dapagliflozin, empagliflozin, and canagliflozin.…
Out Of Pocket Cost For GLP-1 Medications: Planning Tips
Key Takeaways Costs vary by drug, indication, and dose form Cash-pay totals include more than the pen Programs exist, but eligibility is limited Be cautious with compounded versions and unverifiable…
Rural Health Disparities Statistics To Compare Care Gaps
Key Takeaways Define “rural” before comparing outcomes across places. Use age-adjusted rates and stable time windows. Pair health metrics with access and capacity markers. Check small-number limits and data suppression…
DPP-4 Inhibitors Brand Names: Generics, Combos, Tips
Overview If you are sorting medications for type 2 diabetes, names get confusing fast. Lists often mix generics, trademarks, and short-hand. This guide breaks down dpp-4 inhibitors brand names and…