Clinicians and patients often ask, What is Smart Insulin, and how close is it to daily practice. This updated guide explains the science, current devices, and where development is headed next.
Key Takeaways
- Glucose-responsive insulin aims to release insulin only when needed.
- Connected pens track doses, reduce errors, and support safer adjustments.
- CGM integration can inform dosing, but manual confirmation remains essential.
- Oral and patch approaches are in development; most remain investigational.
What is Smart Insulin
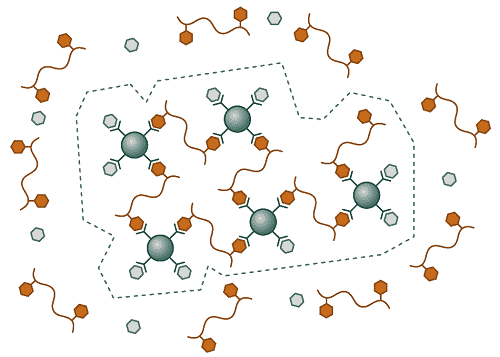
Smart insulin, often called glucose-responsive insulin (GRI), is being designed to activate when glucose rises and to quiet down when it falls. The goal is a tighter physiological response with less hypoglycemia risk. Researchers test polymers, binding motifs, and nanoscale carriers that alter insulin availability as glucose changes. If successful, GRI could simplify dosing and smooth daily variability.
Today’s clinical tools move in that direction using sensors, algorithms, and connected delivery. These systems do not change insulin molecules, but they help the person and care team make more precise timing and dose decisions. For context on broader medication categories and where insulin fits, see Common Diabetes Medications for a structured overview.
How Glucose-Responsive Systems Work
Several designs try to sense glucose and adjust insulin availability. Boronic-acid chemistries, glucose-oxidase reactions, and phenylboronate polymers are common strategies in lab prototypes. These materials may swell, release, or sequester insulin as glucose levels change. Researchers also test microneedle arrays and gel depots that respond quickly, aiming for minute-to-minute sensitivity without overshooting.
Among delivery ideas, a smart insulin patch could release insulin in response to rising glucose on the skin surface. Candidates aim to shorten lag times and avoid large excursions after meals. Bench testing examines response curves, temperature stability, and repeatability across wear cycles. For foundational overviews and definitions that frame these innovations, explore the Diabetes section for concise primers.
Smart Pens and Connected Delivery
Modern pen systems record doses, time stamps, and insulin-on-board, then sync to apps. This helps reduce stacking and missed doses, especially around busy routines. Some models add bolus calculators and reminders, which support safer self-management across age groups. As always, any dose decision should be reviewed with a clinician familiar with your regimen.
The inpen smart insulin pen illustrates how connectivity brings dosing context into one place. Its app can log meals, track active insulin, and share reports with a care team. For rapid- and long-acting delivery examples, see Humalog Kwikpen for a familiar mealtime option, and Lantus Solostar Pens for a basal reference—each linked here to compare device formats and storage thresholds.
Note: Smart features assist decisions but do not replace individualized clinical guidance. Confirm app suggestions against your prescribed plan.
CGM Integration and Data Tracking
Continuous glucose monitoring (CGM) adds context that improves dosing timing and safety. Trend arrows, alerts, and overnight patterns guide decisions like correction doses and snack timing. When data flows into the pen app, the combined view often strengthens adherence and reduces uncertainty during travel or activity changes.
Some ecosystems support direct pairing, such as smart insulin pen dexcom integrations in selected regions. Regulatory pathways vary by market, and features may differ across devices. For urgent highs and sick-day tactics that complement CGM use, see Managing Acute Hyperglycemia for stepwise safety planning. Clinicians also tailor CGM use in autoimmune diabetes; browse Type 1 Diabetes for background on monitoring needs and care coordination.
As interoperability expands, regulators outline expectations for connected safety. For example, the U.S. FDA describes criteria for iCGM systems, including integration controls and labeling, which guide manufacturers developing connected ecosystems. You can review the agency’s description of the Dexcom G6 iCGM system for a concise regulatory snapshot.
Research, Availability, and News
Glucose-responsive formulations remain mostly in preclinical or early clinical testing. Designs must prove consistent activation, minimal lag, and stability during storage and real-world use. Manufacturing scale-up and lot-to-lot reliability are additional hurdles, especially for complex polymer or nanoparticle systems. Peer-reviewed advances appear regularly, yet translation requires rigorous safety data across diverse populations.
People often ask, when will smart insulin be available, but timelines depend on trial outcomes and regulators. Early signals can change as larger studies reveal new challenges. For a broad summary of technology recommendations and safe use principles, review the American Diabetes Association’s technology standards to understand current benchmarks. For patient education resources that complement device adoption, see Diabetes Education Week for practical learning tools and planning tips.
Alternative Pathways: Oral or Patch Approaches
Researchers continue exploring ways to bypass injections. Oral insulin tablets face gastrointestinal barriers, including enzymatic degradation and poor absorption. Approaches include protective coatings, permeation enhancers, and nanoparticle carriers designed to survive the gut and reach the bloodstream. Even with progress, variability remains a central challenge for daily reliability.
Some programs combine enteric protection with absorption boosters, while others target lymphatic uptake to improve bioavailability. Development timelines are hard to predict because dosing precision must match injection standards. Patch-based microneedle arrays are also in testing, with glucose-sensitive materials serving as release gates. For metabolic risk stages often considered in such studies, see Impaired Glucose Tolerance for context on progression and screening.
Choosing a Pen for Daily Use
Selecting a pen starts with the insulin type, dosing needs, and dexterity concerns. Consider display readability, memory functions, and app usability. Training matters too; consistent priming, needle changes, and injection technique can improve accuracy. Clinicians often match device features with lifestyle patterns, like shift work or athletic schedules.
People frequently search for the best insulin pen for type 2 diabetes, but the right choice depends on prescription, dosing flexibility, and support features. Some prefer reusable pens with replaceable cartridges; others prioritize disposable pens for convenience. For a curated view of devices and supplies, explore Diabetes Products to compare form factors and manufacturer instructions side-by-side.
Tip: Keep a simple injection checklist in your app notes. It helps during routine changes or travel days.
Market and Brand Snapshot
Smart pen ecosystems now span multiple manufacturers, with options for reusable and disposable formats. Features can include dose reminders, temperature alerts, and data sharing with care teams. Some systems support cartridge swaps across rapid-acting analogs, while others focus on basal tracking and simplified schedules.
Brand families evolve across regions and may offer pediatric-friendly variants or pen caps with memory functions. As connectivity improves, app ecosystems emphasize clear dose histories and exportable reports. For integrated-dosing tools and pen feature descriptions, manufacturers publish product pages; for example, Medtronic outlines the InPen’s connected features on its InPen overview, which summarizes dose calculators and reporting options.
Cost and Access
Coverage varies widely by plan and region. Consider device cost, sensors (if using CGM), and app or subscription fees when budgeting. A pharmacy team can help parse formularies and identify prior authorization requirements. Some programs provide starter kits or training sessions, which can reduce onboarding time.
When comparing options, search for smart insulin pen price information from the manufacturer and your insurer. Out-of-pocket differences can be substantial between reusable and disposable formats. For type-specific educational materials that may support coverage discussions, browse Type 2 Diabetes for management guides and lifestyle planning resources.
Recap
Smart insulin aims to match the body’s needs more closely, either through responsive molecules or smarter delivery. Connected pens and CGM data already help many users navigate timing and dose decisions. Research continues on oral and patch approaches, with safety and consistency guiding progress. Work with your care team to select devices that match your regimen and daily routine.
For CGM-device interoperability and safety considerations, the FDA’s description of the Dexcom G6 iCGM system outlines integration basics. For current recommendations on diabetes technology, the ADA’s technology standards summarize clinical use, training, and follow-up.
This content is for informational purposes only and is not a substitute for professional medical advice.