Many people ask what is fiasp insulin and how it differs from other rapid-acting options. This guide explains its role, safety profile, dosing principles, device formats, and storage. It also compares Fiasp with similar insulins and outlines practical steps for everyday use.
Key Takeaways
- Ultra-rapid insulin: designed to act faster around meals.
- Multiple formats: FlexTouch pens, Penfill cartridges, and vials.
- Dosing is individualized: timing and amounts vary by regimen.
- Monitor for lows: hypoglycemia remains the most serious risk.
- Storage matters: follow room-temperature limits and discard dates.
What Is Fiasp Insulin
Fiasp is an ultra-rapid formulation of insulin aspart (a rapid-acting analog). It is indicated to improve glycemic control in adults and children with diabetes. Compared with traditional rapid-acting aspart, its formulation includes excipients that speed early absorption. This helps reduce post-meal glucose rises when used with an appropriate meal plan and monitoring routine.
Clinical labeling describes its onset, dosing framework, and major risks, including hypoglycemia. For detailed regulatory information, see the FDA prescribing information for Fiasp, which outlines indications, warnings, and administration details in the product label. Broader guidance on insulin use, targets, and safety is summarized within the ADA Standards of Care, which provide context for clinical decision-making.
For timing concepts across brands, an overview of rapid-acting agents is helpful; see our guide on Rapid-Acting Insulin Peak Time to compare onset and peak windows in one place.
Uses and Indications
Fiasp can be used for prandial (mealtime) coverage and for correction of high glucose values. It is commonly combined with a basal insulin in multiple daily injection regimens. In pump therapy, Fiasp may be used for basal rates and bolus doses if the device and clinical plan support it. Its fast onset suits meal doses given at the start of eating, or in some cases just before.
Healthcare providers individualize its use for type 1 and type 2 diabetes. They consider carbohydrate intake, insulin sensitivity, and concurrent medications. People using carbohydrate counting often match bolus doses to grams of carbohydrate and current glucose trends. Others may apply fixed meal doses with small adjustments based on pre-meal readings.
Side Effects and Safety Considerations
Hypoglycemia (low blood sugar) is the most serious risk with any insulin. Symptoms can include shakiness, sweating, confusion, or dizziness. Severe hypoglycemia may require assistance. Injection-site reactions can occur, including redness, swelling, or itching. Lipodystrophy (fat tissue changes) may develop with repeated injections in the same spot.
Allergic reactions are uncommon but possible. Rotating sites and using appropriate needles can help reduce local reactions. If unusual swelling, widespread rash, or breathing difficulty occurs, urgent evaluation is necessary. The prescribing information lists warnings, precautions, and potential drug interactions. These resources can help contextualize risk when discussing therapy choices with a clinician.
Dosing, Administration, and Timing
Dosing is individualized and depends on the basal-bolus plan, carbohydrate intake, and insulin sensitivity. Many people take meal doses immediately before eating, but some may dose at the first bite or shortly after if intake is uncertain. Correction doses are calculated based on a pre-set sensitivity factor to help bring glucose back toward target. Your plan may evolve as meal patterns and glucose data change.
Counting carbohydrates and understanding insulin-to-carb ratios remain central skills. Continuous glucose monitoring (CGM) can help visualize early glucose changes after dosing. Discuss your ratio, correction factor, and active insulin time with your care team. Small, consistent adjustments guided by logs or CGM trends often improve control while limiting lows.
Devices and Formats
Fiasp is supplied as prefilled pens, cartridges, and vials. The prefilled option is often chosen for convenience and dose accuracy. A Fiasp FlexTouch Pens link is helpful for device specifics and indications, including compatible needles and step-by-step use. Cartridges fit reusable pen devices and allow separate pen choice. Vials support syringe dosing and are commonly used in clinics or pumps when appropriate.
If you prefer reusable pens, see Fiasp Insulin Cartridges for cartridge format details, including volumes and compatibility notes. For syringe users or pump refills, Fiasp Insulin Vials provide a flexible option with standard concentrations. People considering platform alternatives may also review Fiasp vs Humalog for context on formulation and practical differences.
Some patients prefer the simplicity of a fiasp insulin pen for consistent priming and fixed dose increments. Others value the flexibility of cartridges in a favorite reusable pen body. Choose the format that best fits your daily routine, dexterity, and training.
Choosing Between FlexTouch and Penfill
FlexTouch pens arrive prefilled and ready after priming, which can streamline mealtime dosing at work or school. They include audible clicks and consistent force, which helps users with reduced hand strength. Penfill cartridges require a compatible reusable pen and a quick swap when empty. That setup can reduce plastic waste and allows people to keep a preferred pen feel. However, reusable systems require a bit more training, including cartridge changes and device maintenance. Consider your setting, privacy needs, and likelihood of accidental drops when deciding.
Practical Administration Tips
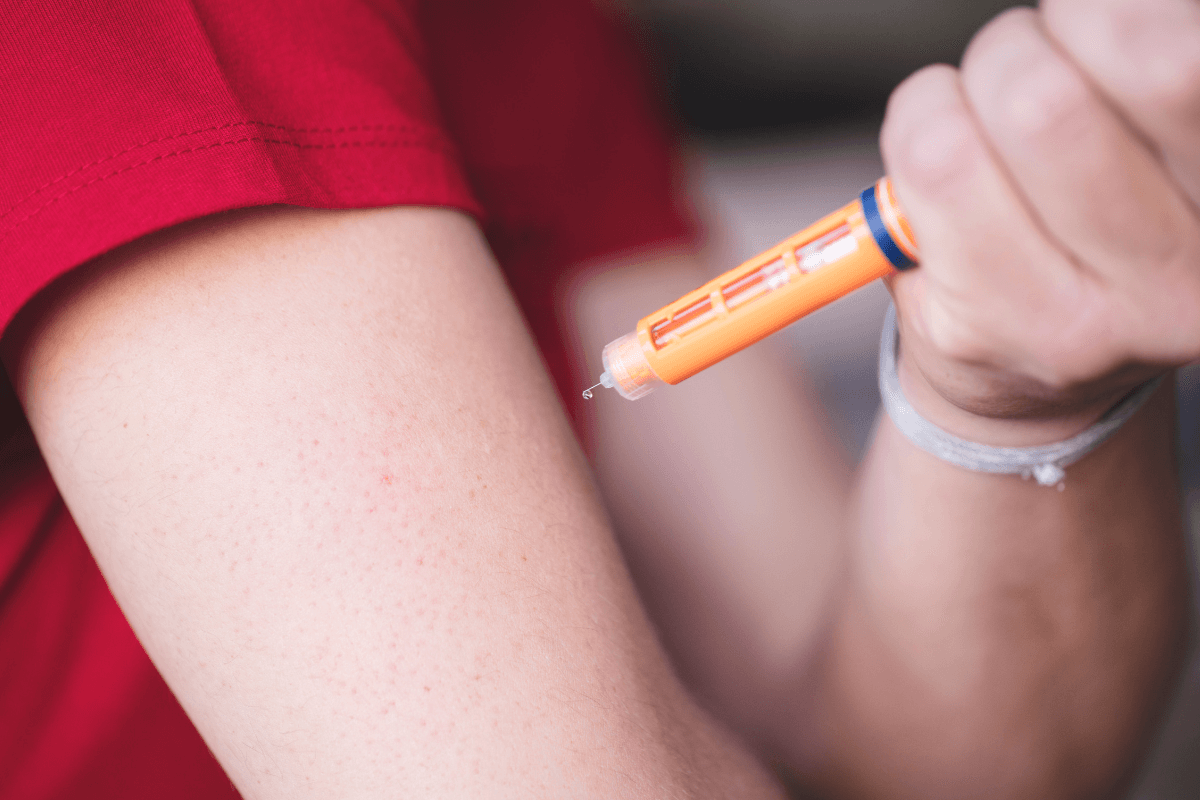
Always prime pens before dosing to ensure a full, accurate bolus. Rotate injection sites across the abdomen, thighs, buttocks, and arms to reduce lipodystrophy. Keep a consistent technique: same depth, angle, and duration under the skin. Recording dose time alongside meals improves retrospective analysis, especially with CGM overlays. If you switch devices, confirm unit increments and maximum dialed dose.
Patients using cartridges often ask about fiasp penfill cartridge how to use. In summary, insert the cartridge into a compatible pen, attach a new needle, prime per manufacturer instructions, and store per label guidance. Replace the cartridge promptly when empty, and discard needles after single use. For active users considering cartridges during exercise blocks, see Fiasp Cartridges for Active Lifestyles for scenario-based tips.
Storage and Stability
Proper storage protects potency. Unopened Fiasp should be kept refrigerated within labeled ranges. Once in use, follow room-temperature limits and discard timelines. People frequently ask how long does fiasp last out of the fridge. Check the device-specific in-use period and temperature threshold, then mark the start date on the pen, cartridge, or vial. Discard the product after the in-use window or if exposed to extremes.
Sun exposure, freezing, and heat can degrade insulin. If the solution looks cloudy or contains particles (and it is not a suspension product), discard it. For broader safety context on viability and handling past labeled dates, see our guide on Expired Insulin, which explains visual checks and discard decisions. Category resources like Diabetes also summarize storage checklists and seasonal considerations.
Travel and Unrefrigerated Use
Travel introduces heat and handling variability. Use insulated carriers, keep insulin out of direct sun, and avoid car glove compartments. During flights, carry insulin in cabin baggage to prevent freezing in the hold. On arrival, store insulin within labeled ranges and continue to track in-use dates. If a bag was exposed to heat or ice packs for long periods, consider replacing the affected device. When in doubt, consult the product label and your care team before continued use.
Tip: Keep a small backup plan. A spare device and glucose tablets can avert emergencies if a pen fails or a dose runs too strong.
Comparisons and Dosing Differences
Comparing rapid analogs helps tailor therapy to routines, sensor data, and meal timing. Discussions often focus on onset, early exposure, and user experience. For example, fiasp vs novolog dosing questions typically revolve around timing relative to meals rather than large dose changes. Some users find earlier dosing with traditional rapid aspart, while others maintain near-start-of-meal dosing with Fiasp. This depends on the meal’s composition and individual absorption.
For brand-to-brand insights, see Fiasp vs Novolog for a structured comparison. If you are evaluating other options, Apidra Alternatives explores another ultra-rapid analog and its clinical context. Our overview on Common Diabetes Medications can help situate prandial insulin within broader diabetes care.
Switching from Other Rapid-Acting Insulins
Switching between brands should be planned with your clinical team. Sensitivity, meal timing, and device differences may change early glucose patterns. When people ask about humalog to fiasp conversion, clinicians often start with unit-for-unit transitions, then adjust timing and ratios based on data. Early follow-up and careful monitoring help refine settings while avoiding hypoglycemia.
Device familiarity also matters. If you move from a KwikPen to a FlexTouch, confirm dose increments and priming steps. For users who prefer equipment continuity, review alternative pens such as Humalog KwikPen and Humalog KwikPen Junior to understand mechanical differences. Those considering vial-and-syringe workflows can compare Humalog Vial setup steps for a complete picture.
Interchangeability with NovoLog
Patients often ask, are fiasp and novolog interchangeable. Both contain insulin aspart, but their formulations differ, which can influence onset and early exposure. Many clinicians avoid calling them directly interchangeable in everyday practice and instead guide a deliberate switch with monitoring. After transition, small timing or ratio adjustments may be needed to match meal patterns and glucose responses.
Some people previously using NovoRapid (international name for NovoLog) report different early glucose behavior when changing to Fiasp. If your meals vary in fat or protein content, timing may need careful reconsideration. For product details and formats to compare, see NovoRapid Cartridge and NovoRapid Vials references included here for device context rather than cost or availability.
Shortages and Access
Supply constraints can disrupt consistent therapy. If a fiasp insulin shortage affects your area, speak with your care team about temporary alternatives in the same class. Some regions have experienced formulary changes or program removals that altered availability. Keep a documented plan for substitutions, including timing adjustments, if you must change quickly.
For a recent example of program impact on access, see our coverage of Fiasp Removal from the PBS, which summarizes implications for Australian patients. If you need a broader view of rapid-acting options during shortages, category pages like Diabetes Products can help you understand format differences when discussing alternatives with a professional.
Recap
Fiasp is an ultra-rapid insulin aspart designed for mealtime and correction use. Its formats offer flexibility, and its early action may help blunt post-meal rises when matched to meal timing. Safe use relies on individualized dosing, careful storage, and prompt monitoring for lows. If switching brands or devices, plan and track results closely to refine settings.
Note: Education, consistent technique, and logs or CGM data often matter as much as the brand itself. Use these tools to make informed adjustments with your care team.
This content is for informational purposes only and is not a substitute for professional medical advice.