Choosing among the dosages of Trulicity requires balancing blood sugar goals, side effects, and practical fit. Trulicity (dulaglutide) is a GLP-1 receptor agonist (hormone-based diabetes drug) used once weekly for type 2 diabetes. Dosing increases gradually to improve tolerance. This overview summarizes strengths, weekly schedules, and when escalation may be considered. Use it to prepare for a focused discussion with your clinician.
Key Takeaways
- Weekly GLP-1 therapy: once-weekly injections simplify adherence.
- Start low, go slow: gradual titration helps limit gastrointestinal effects.
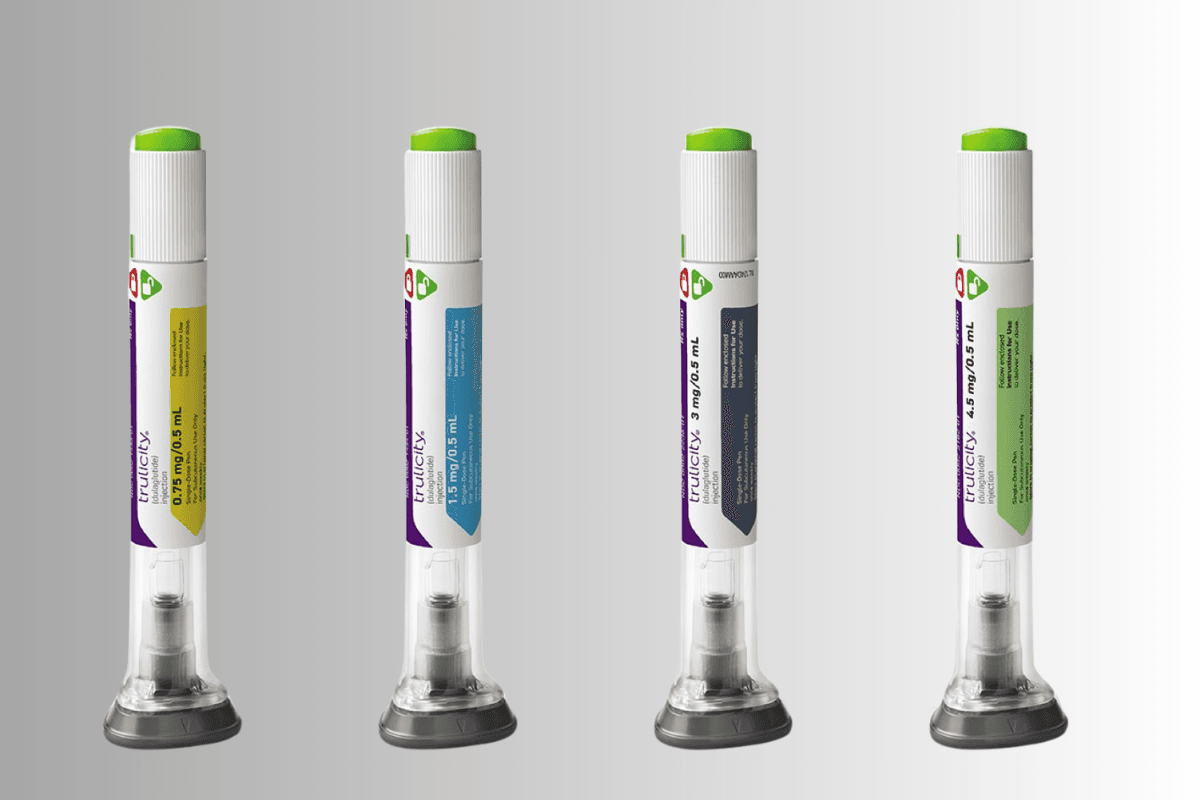
- Four strengths: 0.75 mg, 1.5 mg, 3 mg, and 4.5 mg.
- Dose decisions are individualized based on response and tolerability.
- Missed dose rules and correct injection sites support consistent outcomes.
Dosages of Trulicity: Starting and Titration
Most adults begin with a low weekly dose to limit nausea and gastrointestinal upset. Clinicians reassess after several weeks, then consider stepping up if glucose targets are not met and side effects are manageable. This staged approach can improve persistence and comfort while working toward A1C goals. Trulicity is supplied as single-dose, prefilled pens for once-weekly use.
The weekly schedule is simple: choose a consistent day, and inject on the same day each week. If your day needs to change, keep at least three days between injections. For a fuller overview of schedules and strength availability, see Trulicity Dosage for expanded charts and examples.
Always follow the official instructions and your prescriber’s direction. For complete safety details, the Trulicity Prescribing Information provides labeled guidance on dosing, contraindications, and adverse reactions (Trulicity Prescribing Information).
Dose Strengths: 0.75 mg, 1.5 mg, 3 mg, 4.5 mg
Four strengths allow graduated escalation. The initial dose is generally the lowest. Higher strengths may be considered when fasting or post-meal glucose remain above target, provided side effects are tolerable. As doses increase, some people experience more nausea, reflux, or decreased appetite. In those cases, slower escalation or a step back can help.
The trulicity 0.75 mg dose is commonly used to start therapy and evaluate tolerance. Later increases can be considered based on measured A1C and day-to-day glucose patterns. Pens come as single-use devices, each containing one weekly dose. For device formats and pen-specific details, see Trulicity Pens for an overview of form factors and needle handling.
| Strength | Typical Role |
|---|---|
| 0.75 mg | Starting strength for tolerance and initiation |
| 1.5 mg | First step-up when additional control is needed |
| 3 mg | Second escalation for further A1C lowering |
| 4.5 mg | Highest available strength for select candidates |
How to Increase Safely and Manage Side Effects
Clinicians typically space dose changes by several weeks to track both glycemic response and tolerability. A structured trulicity titration schedule helps limit nausea, early satiety, and reflux. Hydration, smaller meals, and slower eating can reduce queasiness. If gastrointestinal symptoms interfere with daily activities, contact your care team before taking the next injection.
Structured eating and trigger awareness support comfort during escalation. For food-related strategies, see Foods To Avoid With Trulicity for common triggers and practical swaps. If you experience persistent adverse effects, the resource Worst Side Effects Of Trulicity explains when to pause and when to seek care. Professional standards also discuss stepwise escalation and safety; consult the ADA Standards of Care for context on GLP-1 use and monitoring (ADA Standards of Care).
Special Populations and Adjustments
Older adults, those with renal or hepatic impairment, and people with gastrointestinal disorders may need slower progression and closer follow-up. For example, some older adults stabilize at the trulicity 1.5 mg dose if higher strengths worsen appetite or hydration. Kidney disease warrants careful monitoring, especially if vomiting or diarrhea occur. GLP-1 drugs can contribute to temporary dehydration, which may stress kidney function.
Therapy combinations also matter. SGLT2 inhibitors, metformin, or insulin may be co-prescribed with weekly dulaglutide. If kidney protection is a parallel goal, your clinician may also discuss agents used in chronic kidney disease. For context on CKD-focused therapy, see Kerendia for a non-GLP-1 option sometimes used alongside diabetes care plans. For glucose-lowering combinations, Dapagliflozin offers an SGLT2 option often paired with metformin.
Missed Doses, Injection Sites, and Practical Tips
Clear rules reduce confusion and prevent stacking. For missed dose trulicity what to do, inject as soon as you remember if the next dose is at least three days away. If fewer than three days remain, skip the missed dose and take the next dose on the usual day. Do not double up to “catch up.” The official Medication Guide outlines these timing rules in detail (Medication Guide).
Use approved sites: abdomen, thigh, or back of the upper arm. Rotate locations each week to reduce irritation. Review the pen’s instructions before use to confirm priming, needle placement, and disposal steps. For setup visuals and device workflow, see Optimize Trulicity Dose to compare practical techniques that support consistent injections. When appetite changes are strong, Trulicity Weight Loss can help you plan meals and hydration.
Trulicity vs. Ozempic: Dosing Differences
Both are once-weekly GLP-1 therapies, but each has unique dose steps and tolerability patterns. This context matters when switching or comparing alternatives. For example, pens differ in priming, and dose sizes do not map one-to-one. Treatment history, A1C trajectory, and side effect profile guide the choice between molecules.
For a structured head-to-head on escalations and side effects, see Trulicity vs Ozempic for dose steps and clinical considerations. If you are evaluating oral semaglutide, Rybelsus Semaglutide Pills describes a daily alternative with different administration rules. When comparing broader options, Trulicity vs Mounjaro highlights multi-agonist differences relevant to appetite and GI tolerance.
A1C Reduction and Weight Considerations
In general, higher doses may produce additional A1C lowering, balanced against tolerability. Clinicians assess fasting patterns, post-meal spikes, and hypoglycemia risk when deciding next steps. Formal guidelines recommend individualized targets and shared decision-making. For trial summaries and factors that influence response, see Trulicity and A1C Reduction for context and data visuals.
Weight changes can occur with GLP-1 therapy. Appetite suppression varies by person and dose. When outcomes plateau, some teams consider an intermediate step, such as the trulicity 3 mg dose, before evaluating the highest strength. For broader lifestyle support and medication uses, Trulicity Uses outlines indications and practical counseling points.
Recap
Choosing a weekly GLP-1 strength is a stepwise process. Start low, monitor, and increase only when benefits outweigh side effects. Keep injections consistent, follow missed-dose rules, and engage your care team early if problems arise. With a structured plan, weekly therapy can fit smoothly into everyday life.
For broader education, explore Type 2 Diabetes for condition-focused articles and Diabetes for general topics. If you are comparing therapies across classes, Diabetes Products can help you understand available formulations and combination options before your next appointment.
Note: Always use medicines exactly as prescribed and confirmed by your healthcare professional.
This content is for informational purposes only and is not a substitute for professional medical advice.