Understanding insulin resistance vs diabetes helps you act earlier and smarter. These conditions overlap, but they are not the same. Knowing the differences can guide testing, lifestyle changes, and when to seek medical advice.
Key Takeaways
- Core distinction: resistance is an early metabolic defect; diabetes is a diagnosis.
- Testing differs: insulin and glucose dynamics inform risk and disease stage.
- Symptoms often appear late; screening catches problems earlier.
- Diet, activity, sleep, and medications work together for control.
- Track progress with weight, labs, and daily glucose patterns.
Insulin Resistance vs Diabetes: Key Differences
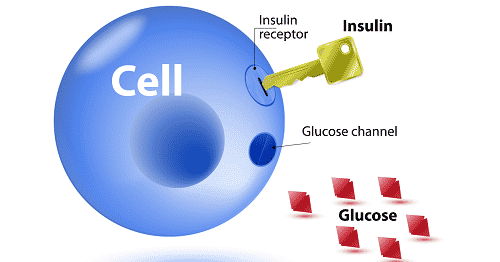
Insulin resistance means the body’s cells respond poorly to insulin, the hormone that moves glucose into tissues. The pancreas compensates by releasing more insulin to hold glucose steady. Over time, this strain may lead to higher fasting glucose, impaired glucose tolerance, and eventually type 2 diabetes.
Diabetes is a clinical diagnosis based on glucose thresholds. Type 2 diabetes often follows years of resistance and beta-cell stress (pancreatic insulin-producing cells). Type 1 diabetes is autoimmune, with absolute insulin deficiency rather than resistance. For a deeper contrast between mechanisms, see Insulin Resistance vs Insulin Deficiency for context on insulin production versus action.
Understanding pancreatic function clarifies these stages. For a focused review of the pancreas and hormone release, see Organ That Produces Insulin to connect anatomy with glucose control.
What Is Insulin Resistance? Definitions and Physiology
Clinically, what is insulin resistance describes a state where normal insulin levels do less than expected. Muscle and liver become less responsive, so the pancreas increases insulin to maintain euglycemia. Early on, blood sugar may stay normal despite elevated insulin. Over months or years, fasting glucose and A1C may drift upward.
At the tissue level, impaired signaling at the insulin receptor and downstream pathways reduces glucose uptake. Chronic excess calories, visceral adiposity, sleep loss, some medications, and genetics can contribute. For molecular background, see Insulin Receptors for how cell signaling affects glucose disposal. Understanding pathways matters because they guide diet and medication choices.
Diagnosing Each Condition: Tests and Thresholds
Clinicians use fasting plasma glucose, A1C, and oral glucose tolerance to diagnose diabetes. An insulin resistance test can include fasting insulin with glucose (e.g., HOMA-IR), a 2‑hour glucose challenge, or more advanced methods like clamp studies used in research. Interpretation should consider age, weight, ethnicity, and comorbidities.
For practical screening, A1C and fasting glucose are widely used. Prediabetes indicates elevated values that do not meet diabetes thresholds. The specific names of tests and panels vary by lab; when comparing any insulin sensitivity panel, review its methodology and reference intervals. For diagnostic ranges and criteria, the American Diabetes Association provides clear cutoffs in its diagnosis standards, which summarize A1C, fasting, and oral glucose thresholds.
Some people ask about home options. While glucose meters and continuous sensors show patterns, a reliable insulin resistance test at home is limited beyond glucose tracking. For a broader overview of hyperglycemia patterns after meals, see Postprandial Hyperglycemia to understand how spikes guide lifestyle changes. For emergency-level high glucose and treatment principles, review What Is Hyperglycemia for safety context.
Diagnostic standards continue to evolve with evidence. For general background on insulin resistance and prediabetes, the CDC overview provides definitions and risk factors in accessible terms. A deeper clinical summary is also available from NIDDK, including prevention strategies supported by trials.
Symptoms and Risk Profiles
Insulin resistance is often silent. Early clues include rising waist size, mild blood pressure elevation, acanthosis nigricans (dark, velvety skin patches), and elevated triglycerides. As glucose rises, people may experience thirst, frequent urination, and fatigue. For classic warning signs related to high glucose, see 3 Ps of Diabetes to recognize thirst, urination, and hunger patterns.
Hormonal changes can shape presentation. Insulin resistance symptoms in females may include irregular periods, acne, hair thinning, or symptoms consistent with polycystic ovary syndrome. Discuss reproductive goals and contraception when planning treatment. Consider family history, sleep disorders, and medications like steroids or some antipsychotics, which may worsen sensitivity.
Nutrition Strategies: Building an Evidence-Informed Plate
Food choices affect insulin needs and glycemic swings. An insulin resistance diet prioritizes minimally processed foods, nonstarchy vegetables, lean proteins, legumes, intact whole grains, nuts, and unsweetened dairy. Many people feel fuller when combining protein, fiber, and healthy fats at each meal.
Carbohydrate quality matters. Emphasize low–glycemic load foods and limit added sugars and refined starches. Some people do best with Mediterranean-style eating; others prefer lower-carb patterns. For detailed meal structures and shopping tips, see Best Diet for Insulin Resistance to translate research into everyday choices.
Use practical tools, not perfection. Keep easy vegetables ready, pre-portion snacks, and plan balanced plates. For stepwise changes that lower risk before diabetes, review Reversing Prediabetes Tips to layer diet, movement, and sleep adjustments.
Medications That May Help
Lifestyle remains foundational, but medications may be added when needed. Metformin for insulin resistance is commonly used to reduce hepatic glucose output and improve sensitivity. It can also support weight-neutral or modest weight-loss effects, which help insulin biology.
Additional drug classes target complementary pathways. SGLT2 inhibitors lower glucose by increasing urinary excretion, while DPP‑4 inhibitors enhance incretin signaling. For an orientation to therapeutic options, see Diabetes Medications Guide to compare mechanisms. If using metformin, review Metformin Dosage for formulation differences and titration principles.
Medication choices should align with cardiovascular risk, kidney function, and patient preferences. Discuss expected benefits, potential side effects, and monitoring. For background on autoimmune versus insulin-resistant conditions, compare pathways in Type 1 vs Type 2 to avoid conflating treatment strategies.
Behavioral Foundations: Activity, Sleep, and Weight
Regular physical activity improves insulin sensitivity in muscle within days. Aim for a mix of aerobic training, resistance work, and light movement breaks during long sitting periods. Sleep duration and quality also matter; short sleep raises hunger hormones and worsens glucose control. Alcohol moderation and stress management further support metabolic stability.
Weight loss, when appropriate, can markedly reduce liver and visceral fat. Even 5–10% loss may lower hepatic insulin resistance and improve fasting glucose. Pair nutrition structure with realistic activity goals to protect adherence. For more reading within type 2 topics, browse Type 2 Diabetes Articles to connect lifestyle themes to labs and outcomes.
Reversal Strategies: From Prediabetes to Better Control
Many people ask how to reverse insulin resistance, and the answer involves consistent habits across diet, activity, sleep, and medications when indicated. Strength training and post-meal walks can reduce glucose peaks. Protein-forward meals with fiber-rich plants curb appetite and support weight control.
Monitoring guides adjustments. Track fasting glucose trends, waist circumference, and weight. Review A1C and lipid profiles with your clinician. For post-meal spikes and pattern interpretation, read Postprandial Hyperglycemia to use readings for targeted changes.
Tracking Improvement: Metrics That Matter
People often look for signs insulin resistance is reversing. Helpful markers include a shrinking waistline, improved triglyceride/HDL ratio, lower fasting insulin (if measured), and steadier post-meal readings. Energy levels, sleep quality, and satiety can also improve as metabolic flexibility returns.
Interpret changes in context. Single readings can vary day to day; look for trends across weeks. Confirm progress with periodic labs and clinical review. For broader glucose safety and symptom recognition, see What Is Hyperglycemia and adjust your plan accordingly.
Related Conditions and Progression
Prediabetes sits between normal glucose and diabetes, often driven by resistance and gradually declining beta-cell function. Without intervention, risk of type 2 rises. Some medications and conditions, such as Cushing’s syndrome or sleep apnea, can worsen sensitivity and should be addressed. Clarify whether patterns suggest deficiency or resistance to guide care.
Symptoms escalate as glucose climbs. Watch for blurred vision, infections, and classic thirst/urination patterns. For early education, the 3 Ps of Diabetes framework can help families recognize changes. For a broad overview of how diet ties into prevention, visit Best Diet for Insulin Resistance to map meals to lab goals.
When to Seek Testing or Care
Consider screening if you have a family history, central weight gain, gestational diabetes history, PCOS, sleep apnea, hypertension, or dyslipidemia. Annual A1C and fasting glucose are common starting points. Additional tests may be added based on risk and prior results. Discuss medications if lifestyle alone does not stabilize glucose.
Urgent symptoms like extreme thirst, frequent urination, nausea, or confusion require prompt evaluation. Review threshold symptoms and next steps in What Is Hyperglycemia for immediate context, and consult your clinician. For a structured medication overview, see Diabetes Medications Guide to understand classes and monitoring.
Recap
Insulin resistance is a metabolic warning sign; diabetes is a diagnosis based on glucose levels. Testing, symptoms, and management differ, but they connect along one continuum. Start with sustainable diet and activity, layer sleep and stress care, and use medications when needed to support physiology and long-term outcomes.
For rounded learning across the site, explore Insulin Resistance vs Insulin Deficiency for mechanism contrasts and Diabetes Medications Guide to align therapies with goals.
Note: Diagnostic and treatment decisions should be made with your licensed healthcare professional, who can personalize testing and options based on your history and preferences.
This content is for informational purposes only and is not a substitute for professional medical advice.