Please note: a valid prescription is required for all prescription medication.
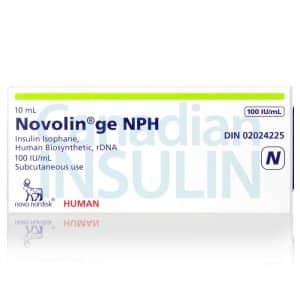
Novolin ge NPH Vial Uses, Safety, and Storage
Also available for your pet.
Offer extended: Use code SAVE10 for 10% OFF all RX meds now through March 10, 2026. Ozempic from Canada and Mounjaro Vial not included. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
$74.99
You save


This product is an intermediate-acting NPH (isophane) human insulin supplied as a vial for injection. Novolin ge NPH Vial is used to help manage glucose levels in people with diabetes. This page explains what it is, how it is typically used, key safety points, and practical handling details.
What Novolin ge NPH Vial Is and How It Works
Novolin ge NPH is a human insulin isophane (NPH) suspension, sometimes called intermediate-acting insulin. After subcutaneous injection, NPH insulin is absorbed more slowly than rapid-acting insulin, so it is often used to support background (basal) insulin needs. Its activity pattern typically includes an onset after injection, a noticeable peak (stronger effect window), and then a decline, which is why timing and monitoring matter. For a broader overview of timing terms across insulin types, see Types Insulin Onset Peak Time Duration.
CanadianInsulin operates as a prescription referral service, not a dispensing pharmacy. Some patients explore Ships from Canada to US as part of their overall access planning, depending on eligibility and jurisdiction. When clinicians discuss basal coverage, they may also compare intermediate-acting options listed under Intermediate Acting Insulin with other basal strategies described in Basal Vs Bolus Insulin.
Because this medicine is a suspension, the insulin particles are not fully dissolved in the liquid. That physical property explains two practical points: it can look cloudy (when mixed properly), and it needs gentle resuspension before each use to help keep dosing consistent. If the liquid remains clumpy, has visible crystals, or does not mix evenly to a uniform cloudy appearance, the vial should not be used and the label guidance should be followed.
People may use NPH insulin as part of a broader diabetes plan that includes nutrition, activity, and glucose monitoring. Background education and condition context are available in the Diabetes Condition overview and the Diabetes Articles hub.
Who It’s For
This insulin is indicated for improving glycemic control in diabetes mellitus when insulin therapy is needed. It may be used in type 1 diabetes and in type 2 diabetes when non-insulin approaches are not enough or are not appropriate. In many care plans, intermediate-acting insulin is used to cover baseline needs, sometimes alongside mealtime insulin. High-level insulin-type comparisons are summarized in Intermediate Acting Insulin Types.
It is not for treating diabetic ketoacidosis (DKA), which is a medical emergency requiring rapid-acting insulin and close monitoring in an acute-care setting. It should not be used during episodes of hypoglycemia (low blood sugar). Anyone with a known serious hypersensitivity to insulin human or to an ingredient in the formulation should avoid it, and seek clinician guidance on alternatives.
Special populations may need additional clinician oversight. Pregnancy, breastfeeding, significant kidney or liver impairment, and older age can change insulin needs and hypoglycemia risk. Intercurrent illness, reduced oral intake, vomiting, and changes in exercise can also affect insulin requirements. These are reasons to plan ahead with a prescriber for sick-day guidance rather than making ad hoc dose changes.
Dosage and Usage
Novolin ge NPH Vial is injected subcutaneously (under the skin) using a U-100 insulin syringe, following the prescriber’s instructions and the product labeling. Dosing is individualized based on factors such as glucose monitoring results, meal patterns, activity, and other diabetes medicines. Intermediate-acting insulin is commonly prescribed once or twice daily, but schedules vary by regimen and clinical goals.
Mixing and administration basics
Because NPH insulin is a suspension, it typically requires gentle mixing before drawing up a dose. The vial is usually rolled between the hands and gently inverted to resuspend insulin evenly; vigorous shaking is generally avoided to reduce foaming and dosing errors. Injection sites are rotated (for example, within the abdomen, thigh, or upper arm) to help reduce lipodystrophy (skin or fat changes that can alter absorption). The technique and device choice can differ from pen-based insulin; a practical comparison is covered in Insulin Pen Vs Syringe.
Quick tip: After mixing, check that the liquid looks evenly cloudy before measuring a dose.
Some regimens combine NPH with other insulins, but whether and how to mix insulins in the same syringe depends on the specific products and the prescriber’s instructions. Insulin products are not automatically interchangeable, even when they share a similar “type.” If a switch is needed, clinicians usually recommend closer glucose monitoring for a period to detect changes in peak timing and overnight lows.
Strengths and Forms
This product is supplied as a U-100 insulin (100 units/mL) vial. In practice, Novolin ge NPH Vial is commonly seen as a 10 mL multidose vial, but packaging and availability can vary by pharmacy and jurisdiction. Always confirm the concentration on the carton and vial label before measuring a dose, and use only U-100 insulin syringes with U-100 insulin to reduce dosing errors.
As a suspension, the insulin should appear uniformly cloudy after proper resuspension. Do not use the vial if you see unusual discoloration, persistent clumps, or particles that do not disperse with gentle mixing. If you are unsure about a vial’s appearance, a pharmacist or diabetes educator can help interpret the label instructions and visual checks.
- Concentration: U-100 (100 units/mL)
- Form: NPH insulin suspension
- Route: Subcutaneous injection
- Device: Vial with syringe
For additional browsing across insulin presentations and classes, the Insulin Products category can be used to compare forms (vials, pens, cartridges) and types.
Storage and Travel Basics
Store insulin exactly as described in the product labeling. In general, unopened insulin is kept refrigerated and protected from light, and it should not be frozen. Do not use insulin that has been frozen, overheated, or exposed to direct sunlight for prolonged periods. Keep the vial in its carton when possible to reduce light exposure and mix-ups.
Once a vial is in use, labeling often allows storage at controlled room temperature for a limited time, but the exact conditions and discard timeline can differ by product and region. Check the carton insert and pharmacy label for the in-use window, and write the date opened in a consistent place so it is easy to track. Storage mistakes are a common cause of unexpected glucose variability; the practical risks are reviewed in Improper Insulin Storage Dangers.
For travel, plan for temperature protection and access to supplies. Insulin should not touch ice packs directly, which can freeze it. Carry syringes, glucose testing supplies, and a backup plan in case of delays. If you use a continuous glucose monitor or pump for other parts of therapy, confirm with your clinician how intermediate-acting insulin fits into the overall plan.
Side Effects and Safety
The most important risk with any insulin is hypoglycemia. Symptoms can include sweating, shakiness, hunger, headache, confusion, irritability, and fast heartbeat. Severe hypoglycemia can cause seizures or loss of consciousness and needs urgent treatment. Because intermediate-acting insulin can peak hours after dosing, some people are more likely to notice lows between meals or overnight depending on their schedule.
Why it matters: Recognizing early low-glucose symptoms can help prevent progression to severe hypoglycemia.
Other possible effects include weight gain, injection-site reactions (redness, swelling, itching), and lipodystrophy with repeated injections in the same area. Rare but serious allergic reactions can occur, including generalized rash, breathing difficulty, or swelling of the face or throat; emergency care is required if these occur. Insulin can also lower potassium (hypokalemia), which can be clinically significant in people using diuretics or with certain heart conditions.
Monitoring plans vary. Clinicians may recommend periodic review of glucose logs or CGM trends, A1C testing, and evaluation of hypoglycemia awareness. If episodes of low glucose become more frequent, or if you have reduced ability to sense lows, bring this to the prescriber’s attention so the overall regimen can be reassessed.
Drug Interactions and Cautions
Many medicines and health conditions can change insulin needs. Some drugs may increase hypoglycemia risk (for example, other glucose-lowering agents), while others may raise glucose levels and lead to higher insulin requirements (for example, corticosteroids). Alcohol can also contribute to hypoglycemia, especially when intake is not accompanied by food.
Beta-blockers can mask some symptoms of hypoglycemia, such as tremor and palpitations, making low glucose harder to recognize. ACE inhibitors, salicylates, and some antidepressants can also affect glucose control in certain people. Thiazide diuretics, thyroid hormones, and some antipsychotics may raise glucose levels. This is not a complete list, so it is important that a clinician or pharmacist reviews all prescription medicines, over-the-counter products, and supplements for potential effects on glucose.
Caution is also warranted with changes in routine. Shifts in meal timing, reduced appetite, new exercise plans, and acute illness can change the balance between insulin and glucose intake. Driving or operating machinery requires special attention because hypoglycemia can impair reaction time; clinicians often advise checking glucose more frequently if you have had recent lows.
Compare With Alternatives
Intermediate-acting NPH insulin is one option for basal coverage. Other basal insulins are longer-acting analogs (for example, insulin glargine or insulin degludec), which typically have a flatter activity profile and less pronounced peak than NPH. Some people use rapid-acting insulin at meals (bolus) plus a basal insulin, while others use premixed products that combine intermediate and short/rapid components. The best fit depends on meal patterns, hypoglycemia history, monitoring approach, and clinician preference.
Device and formulation differences also matter. Vials require syringe technique and consistent resuspension for cloudy suspensions, while many long-acting analogs are clear solutions in pens. For examples of other insulin presentations, clinicians may reference products such as Novorapid Cartridge for mealtime dosing or Lantus Solostar Pens for basal coverage, depending on the prescribed regimen.
Switching between insulin types is not a simple like-for-like substitution. Even when the total daily units look similar, onset, peak, and duration can differ and change the timing of lows and highs. If a change is being considered, it is usually paired with a monitoring plan and a clear set of thresholds for when to contact the prescriber.
Pricing and Access
Novolin ge NPH Vial requires a valid prescription in most jurisdictions. Coverage and out-of-pocket costs can vary based on your drug plan, deductible status, pharmacy channel, and whether a biosimilar or alternative insulin is considered equivalent for your plan’s purposes. For people without insurance, cash-pay considerations may include pharmacy dispensing fees, vial quantity, and any required supplies such as U-100 syringes and sharps containers.
When needed, prescription details are confirmed with the prescriber before processing. Access may also involve cross-border fulfilment considerations, such as identity verification, appropriate documentation, and local rules about importation for personal use. Educational updates and stable informational listings may appear on the Promotions page, but eligibility and availability can change and should be verified at the time of review.
Dispensing is handled by licensed third-party pharmacies where permitted. If a regimen includes multiple insulins, it can help to keep a current medication list that includes product names, concentrations (such as U-100), and administration devices. This supports safer reconciliation when a clinician changes therapy, when a pharmacy substitutes a presentation, or when a patient travels.
Authoritative Sources
For labeling and product identification basics, consult DailyMed resources: https://dailymed.nlm.nih.gov/dailymed/.
For patient-friendly NPH insulin information, review MedlinePlus insulin isophane guidance: https://medlineplus.gov/druginfo/meds/a682611.html.
For practical insulin storage principles, see the American Diabetes Association overview: https://diabetes.org/healthy-living/medication-treatments/insulin-other-injectables/insulin-storage-and-syringes.
For temperature-sensitive medications, packaging and prompt, express, cold-chain shipping may be used to help maintain stability in transit.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is NPH insulin and how is it different from rapid-acting insulin?
NPH (isophane) insulin is an intermediate-acting insulin designed to provide background glucose-lowering support for part of the day or night. Compared with rapid-acting insulin, it generally starts working later, has a more pronounced peak effect, and lasts longer. Rapid-acting insulin is typically used to address mealtime glucose rises, while NPH may be used for basal needs or in certain mixed regimens. The right combination and timing depend on a prescriber’s plan and your monitoring data.
Why does this insulin look cloudy, and when should I not use it?
NPH insulin is a suspension, which means insulin particles are mixed throughout the liquid rather than fully dissolved. After gentle mixing, it should look uniformly cloudy. Do not use the vial if you see clumps that do not disperse, crystals stuck to the container, unusual discoloration, or anything that looks inconsistent with the labeling instructions. If you are unsure, ask a pharmacist or clinician to review the vial’s appearance and storage history before using it.
How do I recognize and respond to low blood sugar while using NPH insulin?
Low blood sugar (hypoglycemia) may cause sweating, shakiness, hunger, headache, fast heartbeat, confusion, or irritability. Severe episodes can lead to seizures or loss of consciousness and require urgent help. Because NPH can peak hours after dosing, some people notice lows between meals or overnight. Follow your clinician’s plan for monitoring and treatment, including when to use fast-acting carbohydrates or glucagon if prescribed. Tell your prescriber if lows are frequent or symptoms are hard to feel.
Can I mix NPH insulin with other insulin in the same syringe?
Some regimens use mixed insulins, but mixing rules depend on the specific products involved and the prescriber’s instructions. In some cases, NPH may be mixed with short-acting insulin, but other combinations are not recommended, and technique matters to avoid altering absorption. Never assume two insulins can be combined just because they are both U-100. If mixing is part of your plan, ask for written steps that cover preparation order, timing of injection, and how to avoid contamination between vials.
What should I ask my clinician before switching from NPH to another basal insulin?
Ask how the new insulin’s onset, peak, and duration differ, and what that means for dosing time and hypoglycemia risk. Clarify whether the total daily units are expected to change and how to monitor during the transition. It also helps to ask about sick-day instructions, what to do if a dose is missed, and how to adjust glucose checks temporarily. If you use other diabetes medications, confirm whether any need changes at the same time to reduce unexpected highs or lows.
How should I store an in-use insulin vial during daily life or travel?
Follow the product label for storage limits and discard timelines. In general, insulin should be protected from freezing, high heat, and direct sunlight. Keep it in its original packaging when practical, and avoid leaving it in a hot car or near heating vents. For travel, use an insulated bag and keep insulin from touching ice packs directly to prevent freezing. If you suspect temperature damage or see unusual appearance after mixing, seek pharmacist guidance before continuing use.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
Ozempic Side Effects In Females: Symptoms, Risks, Next Steps
Overview Ozempic (semaglutide) is a GLP-1 receptor agonist medication used for type 2 diabetes. Some people also discuss it in the context of weight management. This article focuses on ozempic…
Zepbound Side Effects Long-Term: What to Monitor Over Time
Key Takeaways Most effects are gastrointestinal and often improve over time. You may notice symptoms soon after the first injection. Track patterns: timing, triggers, and recovery after each dose. zepbound…
GLP-1 Drugs for Weight Loss: Options, Risks, and Next Steps
Key Takeaways These medicines target appetite signals and digestion to support weight management. Approval and use vary by product, condition, and country-specific labeling. Many options are injections; one GLP-1 medicine…
SGLT2 Inhibitors Mechanism of Action in Heart Failure
Overview Heart failure is not just a “weak heart.” It is a body-wide syndrome that affects fluid balance, kidneys, and energy use. Understanding sglt2 inhibitors mechanism of action in heart…