Please note: a valid prescription is required for all prescription medication.
Humalog Cartridge Uses, Safety, and Storage
Offer extended: Use code SAVE10 for 10% OFF all RX meds now through March 10, 2026. Ozempic from Canada and Mounjaro Vial not included. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
$97.99
You save


Humalog Cartridge is a cartridge form of insulin lispro used to help manage glucose in diabetes. This page explains how cartridges are used with compatible reusable insulin pens, along with safety and storage basics. It also acknowledges that many people compare Humalog Cartridge price while planning ongoing treatment discussions.
What Humalog Cartridge Is and How It Works
Humalog Cartridge contains insulin lispro, a rapid-acting insulin analog (a lab-made insulin designed to act quickly). It helps move glucose from the bloodstream into cells and reduces glucose production by the liver. For many people, it is used around mealtimes to address post-meal glucose rises as part of a broader plan that may also include a longer-acting (basal) insulin.
CanadianInsulin operates as a prescription referral service and may confirm prescription details with the prescriber when required. Some patients explore US delivery from Canada as a cross-border fulfilment option, depending on eligibility and jurisdiction. Cartridge products are typically intended for injection with certain reusable pens, and they are not the same as vials used with syringes.
Rapid-acting insulins are generally taken close to meals because they begin working relatively soon after injection. The exact onset, peak effect, and duration can vary by person, dose, injection site, activity, and meal composition. For background context on how different insulins behave over time, the guide Types Insulin Onset Peak summarizes common patterns clinicians reference.
Dispensing is handled by licensed third-party pharmacies where permitted under applicable rules. When reviewing Humalog Cartridge price comparisons, it can help to separate the medication’s clinical role (rapid mealtime insulin) from the separate question of how the cartridge form fits your device setup and prescription details.
Who It’s For
This medicine is used to improve glycemic control in people with diabetes mellitus, when insulin is indicated. It may be part of care plans for both Type 1 diabetes and Type 2 diabetes, including combination regimens that use multiple medication classes. For condition-level background and related options, you can browse the Type 1 Diabetes hub or the Type 2 Diabetes article collection.
Humalog Cartridge may be considered when a clinician wants a rapid-acting insulin delivered via a reusable pen that accepts cartridges. Suitability depends on the full regimen, the patient’s ability to use the device correctly, and factors such as hypoglycemia risk and meal timing. In pediatrics or older adults, additional supervision and monitoring may be needed, especially during regimen changes.
It should not be used during episodes of hypoglycemia (low blood glucose). It is also contraindicated for people with known hypersensitivity to insulin lispro or any component of the formulation. If there has been a prior serious allergic reaction to an insulin product, a prescriber may review ingredients and consider alternatives or additional precautions.
People who have recurrent severe hypoglycemia, reduced hypoglycemia awareness, significant kidney or liver impairment, or irregular meal patterns may require closer follow-up. These considerations do not automatically rule out use, but they often affect how the overall plan is structured and how monitoring is performed.
Dosage and Usage
Dosing for insulin is individualized by the prescriber. Rapid-acting insulin is commonly used in relation to meals, and it may also be used for correction dosing based on a clinician-provided plan. Do not change dose, timing, or insulin type without prescriber guidance, since small changes can meaningfully affect glucose control and hypoglycemia risk.
Humalog Cartridge price comparisons sometimes lead people to switch between presentation types (for example, pen cartridges versus prefilled pens or vials). If a switch is being considered, the prescriber typically confirms that the concentration, device method, and administration instructions match the intended prescription. The article Insulin Pen Vs Syringe reviews practical differences that can matter for technique and supplies.
Cartridge use is tied to device compatibility. Before first use, read the pen and cartridge instructions so the cartridge is seated correctly, the needle is attached safely, and priming steps are completed according to the device directions. Injection technique usually includes site rotation (changing locations within the recommended areas) to help reduce skin thickening and variable absorption.
Quick tip: Keep a consistent routine for site rotation to reduce lipohypertrophy (fatty tissue thickening).
Some people also use diabetes technology like continuous glucose monitoring (CGM) or connected pens. These tools can support pattern recognition, but they do not replace clinical instructions on dosing. The overview Understanding Diabetes Tech provides context on how pens, pumps, and CGMs may fit together.
Strengths and Forms
Humalog Cartridge is a pen cartridge presentation of insulin lispro. The product page title indicates a U-100 concentration (100 units/mL). Cartridges are designed for use in compatible reusable insulin pens that accept this cartridge format; compatibility depends on the pen model and manufacturer guidance.
Cartridges are often associated with a 3 mL fill volume, but packaging and presentation details can vary by market and pharmacy. If your care plan depends on a specific cartridge volume or box count, confirm those details on the dispensing label and carton before use. Your clinician or pharmacist can also help confirm whether your current pen body is suitable for the cartridge system you have.
| Attribute | What to confirm |
|---|---|
| Concentration | U-100 (100 units/mL) on the label |
| Presentation | Cartridge for a compatible reusable pen |
| Supplies | Pen needles, sharps container |
When selecting supplies, be sure the needle type and length are appropriate for the pen and patient needs. People who need help navigating insulin categories and related products can browse the Diabetes Medications Insulin product hub to see other insulin presentations and formats.
Storage and Travel Basics
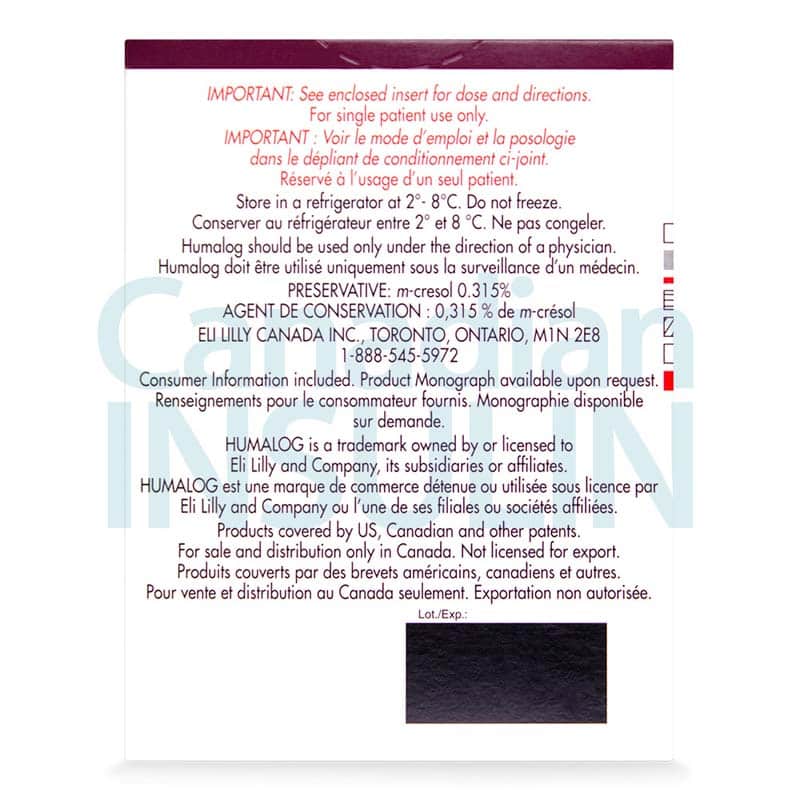
Insulin is temperature sensitive. Unopened cartridges are typically stored in a refrigerator and should not be frozen. Avoid placing insulin directly against freezer packs or cooling elements, since freezing can damage the protein and make dosing unreliable. Once in use, many insulin products can be kept at controlled room temperature for a limited time, but the specific timeframe depends on the labeled instructions for that exact product and presentation.
Do not use cartridges that look unusual (for example, unexpected particles or discoloration), and avoid using insulin past the labeled expiration date. If you are unsure whether a cartridge has been overheated or frozen, a pharmacist can advise whether it should be replaced. For deeper handling guidance, the resource Insulin Storage Best Practices outlines common do’s and don’ts.
When traveling, plan for temperature control, backups, and documentation. Carry insulin and supplies in a carry-on bag when flying, and keep a copy of the prescription or clinic note if required by your destination or airline. The article Traveling With Diabetes covers practical preparation steps and common pitfalls.
Why it matters: Heat exposure can reduce potency and make glucose control less predictable.
When comparing Humalog Cartridge price, also consider wastage risk from improper storage, since replaced insulin adds burden even when coverage is available.
Side Effects and Safety
The most common and clinically important risk with insulin is hypoglycemia. Symptoms can include shakiness, sweating, hunger, headache, confusion, or irritability, and severe episodes can lead to seizures or loss of consciousness. People at higher risk include those with missed meals, unexpected activity, alcohol use, recent dose changes, or reduced kidney function. Ongoing glucose monitoring helps detect patterns that can be discussed with the prescriber.
Other possible effects include injection-site reactions (redness, swelling, itching), lipodystrophy (skin or fat changes where injections occur), weight gain, and peripheral edema (swelling). Rarely, serious allergic reactions can occur and require urgent care. Low potassium (hypokalemia) is an uncommon but potentially serious risk with insulin therapy, particularly in people with predisposition or with certain interacting medicines.
Humalog Cartridge price research should not distract from confirming safety basics: how to recognize and treat low glucose, when to seek urgent help, and how to avoid common technique errors. If a person has reduced awareness of hypoglycemia, the care team may discuss extra monitoring, regimen simplification, or technology supports.
If symptoms are severe, rapidly worsening, or accompanied by fainting, chest pain, or breathing difficulty, seek emergency care. Report suspected allergic reactions, repeated severe lows, or persistent injection-site problems to a clinician promptly, since these issues may require changes to the overall plan or the injection approach.
Drug Interactions and Cautions
Many medicines and supplements can affect glucose levels or the body’s response to insulin. Some drugs may increase hypoglycemia risk, while others can raise glucose and increase insulin needs. Beta-blockers can also mask some hypoglycemia warning signs (such as tremor or palpitations), making monitoring and pattern awareness more important.
Examples of interacting or cautionary categories include corticosteroids, thyroid hormones, some antipsychotics, diuretics, and certain HIV therapies. Alcohol can also increase hypoglycemia risk, especially when combined with missed meals. If you are using other glucose-lowering agents, a prescriber may coordinate how they fit with insulin to reduce overlapping risk. The overview Common Diabetes Medications describes several classes that are often used alongside insulin.
Thiazolidinediones (TZDs) used with insulin may increase the risk of fluid retention and heart failure in susceptible patients. Kidney or liver impairment may also change insulin sensitivity. Always share an updated medication list with the care team, including over-the-counter products, and follow the specific instructions for your pen device and needle disposal.
If a person is ill, eating less, or experiencing vomiting or dehydration, glucose can become harder to predict. Sick-day plans are individualized, so it helps to have written instructions from the clinician for when to check glucose or ketones and when to seek medical care.
Compare With Alternatives
Rapid-acting insulin options are not interchangeable without prescriber direction, even when they are in the same broad category. Differences can include device format, labeled interchangeability, and how the regimen is written. Some people discuss other rapid-acting analogs (such as insulin aspart or insulin glulisine) with their clinician, particularly if they need a different device ecosystem or have specific formulary constraints.
In many regimens, a rapid-acting insulin is paired with a basal insulin. Basal options include insulin glargine and insulin detemir, which have different timing profiles than mealtime insulin and are used for background coverage. For readers comparing basal products, the educational piece Humulin Vs Lantus summarizes how intermediate-acting and long-acting insulins differ in typical use.
If your plan involves a reusable pen system, cartridge formats may also matter. For examples of other cartridge-based basal products that some people use in combination regimens, see Lantus Cartridges and Levemir Penfill Cartridges. These are different insulins and should only be compared with clinician input.
When evaluating alternatives, confirm three basics with the care team: insulin type (rapid vs basal), concentration, and device compatibility. Switching the wrong component can increase hypoglycemia risk or leave gaps in coverage.
Pricing and Access
Access to insulin cartridges typically requires a valid prescription. Documentation requirements vary by jurisdiction, and the prescription needs to match the intended presentation (cartridge versus vial or prefilled pen). Coverage and out-of-pocket responsibility can differ widely across plans and regions, so patients often review benefits, prior authorization rules, and preferred product lists before changing forms.
For people comparing Humalog Cartridge price, common drivers include plan design, pharmacy network rules, quantity limits, and whether a person needs the cartridge format for a reusable pen. For patients without insurance, cash-pay considerations may include the specific presentation chosen and the need for compatible pen supplies. If you are gathering background information on options and policies, Programs And Updates may provide general updates without substituting for insurer benefits details.
Cross-border fulfilment options vary by jurisdiction and patient eligibility. In this operating model, referrals help route prescription information, while a licensed dispensing pharmacy completes the final check and provides the medication where permitted. If any prescription details are unclear, the process may include confirming information with the prescriber before dispensing proceeds.
It can also help to plan for continuity: keep an eye on remaining supply, store products correctly, and have a plan for travel or emergencies. When fulfilment is arranged, temperature-sensitive packages may use prompt, express, cold-chain shipping based on pharmacy protocols and product requirements.
Authoritative Sources
For the most reliable details on indications, contraindications, and administration instructions, consult the official prescribing information for the exact insulin lispro product and presentation you have. Device instructions for the specific reusable pen are also important, since cartridge loading and priming steps can differ by model. If anything on a carton label conflicts with what you were told, confirm with a pharmacist or prescriber before using the cartridge.
The resources below are useful starting points for label-level details and general diabetes guidance. They are not a substitute for individualized medical advice, but they can help you prepare questions for a clinician and understand standard safety warnings.
For U.S. label details, review the DailyMed database of FDA label information.
For standards of care context, see the American Diabetes Association guidance and patient resources.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is the difference between an insulin cartridge and a vial?
An insulin cartridge is designed to be inserted into a compatible reusable insulin pen body, while a vial is typically used with a syringe (or sometimes to fill a pump reservoir, depending on the insulin and device). Cartridges can be convenient for people who prefer a reusable pen system and want to replace only the cartridge when it is empty. A vial may be more flexible for syringe-based dosing. The correct choice depends on the prescription, device compatibility, and the technique you and your clinician have selected.
Can Humalog cartridges be used in any reusable insulin pen?
No. Cartridge compatibility depends on the pen model and the cartridge system it was designed to accept. Even if two cartridges look similar, they may not fit or function safely in a specific pen. Before using a cartridge, confirm the pen brand/model and follow the pen manufacturer’s instructions for loading, priming, and needle attachment. If you are unsure, a pharmacist can help verify whether your pen is intended for that cartridge type and whether any adapters are required.
How quickly does insulin lispro work, and when is it usually taken?
Insulin lispro is generally considered rapid acting, meaning it starts lowering glucose relatively soon after injection and is often used around mealtimes. Exact timing depends on the individual plan written by the prescriber, meal composition, activity, and glucose trends. Because timing is part of the dosing plan, it is important not to change when you take it without clinical guidance. If you are seeing unexpected highs or lows, bring glucose logs or CGM reports to your next visit.
What side effects should be monitored most closely with Humalog?
Hypoglycemia is the key risk to monitor with any insulin therapy. Track symptoms such as shakiness, sweating, confusion, or unusual fatigue, and follow your clinician’s instructions for treating low glucose. Also watch for recurring injection-site irritation and skin changes such as lumps or thickening, which can affect absorption. Seek urgent care for severe allergic symptoms (trouble breathing, facial swelling, widespread hives) or for severe low glucose causing loss of consciousness or seizures. Report repeated severe episodes to your prescriber.
How should Humalog cartridges be stored during travel or a power outage?
Insulin should be protected from temperature extremes. During travel, keep cartridges with you rather than in checked luggage, and avoid leaving them in a hot car or against freezing packs. For short disruptions at home, the safest approach is to follow the storage instructions on the carton and avoid freezing. If you suspect insulin has been overheated or frozen, potency may be reduced even if it looks normal. When in doubt, confirm with a pharmacist and consider replacing the affected supply.
What should I ask my clinician before switching insulin types or presentations?
Ask whether the new product is the same insulin type (rapid vs basal), the same concentration (for example, U-100), and the correct presentation (cartridge, vial, or prefilled pen). Confirm how timing around meals should work, what to do for missed meals or exercise, and how to handle sick days. If you use a reusable pen, ask about cartridge compatibility and priming steps. It also helps to review how to recognize and treat hypoglycemia and when to seek urgent care.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
Zepbound Side Effects Long-Term: What to Monitor Over Time
Key Takeaways Most effects are gastrointestinal and often improve over time. You may notice symptoms soon after the first injection. Track patterns: timing, triggers, and recovery after each dose. zepbound…
GLP-1 Drugs for Weight Loss: Options, Risks, and Next Steps
Key Takeaways These medicines target appetite signals and digestion to support weight management. Approval and use vary by product, condition, and country-specific labeling. Many options are injections; one GLP-1 medicine…
SGLT2 Inhibitors Mechanism of Action in Heart Failure
Overview Heart failure is not just a “weak heart.” It is a body-wide syndrome that affects fluid balance, kidneys, and energy use. Understanding sglt2 inhibitors mechanism of action in heart…
DPP-4 Inhibitors Weight Loss: What Research Shows Clinically
Key Takeaways DPP-4 inhibitors usually have little effect on body weight. Most studies describe this class as “weight neutral,” not weight-loss therapy. Weight change often depends more on diet, activity,…