Please note: a valid prescription is required for all prescription medication.
Lucentis Vial Uses, Safety, and Storage
Offer extended: Use code SAVE10 for 10% OFF all RX meds now through March 10, 2026. Ozempic from Canada and Mounjaro Vial not included. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
$2,413.99
You save


Lucentis is a prescription medicine containing ranibizumab, used in the eye to treat certain retinal diseases that can threaten vision. It is given as an intravitreal injection (an injection into the gel inside the eye) by trained eye-care professionals. This page summarizes what to know about Lucentis Vial, including how it works, dosing basics, safety, and storage.
Because retinal conditions and treatment plans vary, the most relevant details usually come from the prescribing information and your retina specialist’s clinical plan.
What Lucentis Is and How It Works
Ranibizumab is an anti-VEGF medicine (it blocks vascular endothelial growth factor, a signal that can drive abnormal blood vessel growth and leakage in the retina). By reducing VEGF activity in the eye, this treatment may help limit fluid buildup and bleeding that can damage central vision. The medicine is delivered directly into the eye, which concentrates the effect locally while keeping systemic exposure relatively low compared with intravenous drugs.
Some patients explore US shipping from Canada when cross-border fulfilment is permitted for their situation. For access workflows that involve CanadianInsulin, prescription details may be verified with the prescriber before a referral is completed, and the medication may be dispensed by appropriately licensed partner pharmacies where permitted.
In practice, ranibizumab is used within retina clinics that monitor vision, retinal imaging (such as optical coherence tomography), and injection-related safety. Treatment is often part of a longer-term plan, since many retinal diseases are chronic or prone to recurrence.
Why it matters: Anti-VEGF therapy targets a key driver of retinal swelling and vessel leakage.
To explore related eye-care medication areas and clinic-use products, you can browse the Ophthalmology Product Category and the Ophthalmology Articles hub for general context.
Who It’s For
Lucentis Vial is used for several retinal disorders where abnormal blood vessels or fluid leakage threaten sight. Indications can include wet age-related macular degeneration, diabetic macular edema, macular edema following retinal vein occlusion, myopic choroidal neovascularization, and certain pediatric retinal conditions per labeling and specialist care pathways.
Condition context may be helpful if you are learning the terminology used in clinic notes. CanadianInsulin maintains browseable condition hubs such as Wet Age Related Macular Degeneration, Diabetic Macular Edema, Macular Edema From Retinal Vein Occlusion, Myopic Choroidal Neovascularization, and Retinopathy Of Prematurity.
This medicine is not appropriate for everyone. Clinicians generally avoid intravitreal anti-VEGF injections in eyes with active ocular or periocular infection, and they use added caution if there is significant intraocular inflammation. A history of hypersensitivity to ranibizumab or formulation components is also a key concern. Your ophthalmology team will weigh eye findings, overall health, pregnancy considerations, and the urgency of vision preservation when deciding on therapy.
Dosage and Usage
Dosing for Lucentis Vial depends on the condition being treated, the patient population, and the prescriber’s plan. Many adult retinal indications use a small fixed injection volume delivered into the vitreous cavity at intervals defined in the prescribing information (often monthly at the start, with interval adjustments based on response and monitoring). Some indications may use different dose amounts or schedules, and pediatric dosing may differ from adult dosing.
The injection is performed under aseptic technique (sterile preparation) in a clinical setting. The eye is numbed, the ocular surface is disinfected, and the medicine is injected using specialized technique to reduce contamination risk. Afterward, clinicians may check for immediate complications such as elevated intraocular pressure and may provide guidance on short-term activity precautions.
Clinic administration overview
Intravitreal injections are typically performed by retina specialists or trained ophthalmology clinicians. The vial is intended for single use, and the dose is prepared using sterile supplies and a controlled workflow. Patients are usually counseled about expected short-term symptoms (mild irritation, tearing, a scratchy sensation) versus warning signs that need urgent evaluation. Monitoring often includes vision testing and retinal imaging at follow-up visits, since the goal is to control retinal fluid and preserve function over time.
Quick tip: If you keep a symptom log, note which eye was treated and when.
If you want a general refresher on how “mechanism of action” explanations are structured across medicines, one example resource is Actos Work; the concepts of targets and downstream effects are similar even when diseases differ.
Strengths and Forms
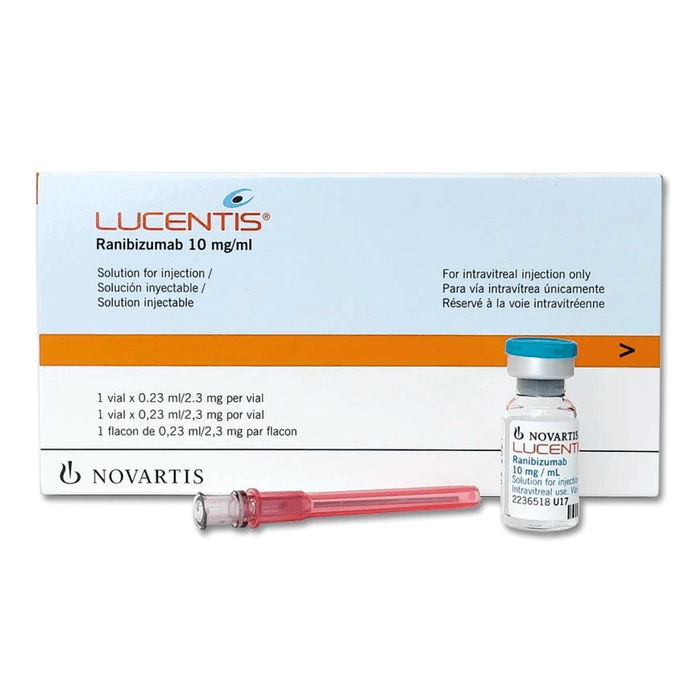
Lucentis is supplied in different presentations, and availability may vary by jurisdiction and pharmacy channel. Lucentis Vial commonly refers to a single-use vial containing ranibizumab at a labeled concentration intended for intravitreal injection. In some settings, a prefilled syringe presentation may also be available, which can reduce certain preparation steps in clinic workflows.
The product information on your specific vial or carton is the best source for the exact concentration and fill volume. Many listings describe the vial as 10 mg/mL with a fill volume that supports withdrawal of a small intravitreal dose, with excess volume present to allow for preparation and priming according to labeling.
| Presentation | What it is | Typical setting |
|---|---|---|
| Single-use vial | Vial used to withdraw an intravitreal dose | Retina clinic or hospital use |
| Prefilled syringe | Manufacturer-prepared syringe for injection | Retina clinic workflows |
When comparing formats, clinicians focus on sterile handling steps, dosing accuracy, and inventory management rather than patient self-administration, since the injection is not intended for at-home use.
Storage and Travel Basics
Store ranibizumab products exactly as labeled. In general, Lucentis should be refrigerated and protected from light, and it should not be frozen. Avoid shaking, since vigorous agitation can affect protein-based medicines. Keep the product in the original carton until use to reduce light exposure and to keep identifying information with the medication.
For clinic transport or travel between sites, the goal is temperature control and protection from physical damage. Use an insulated container and follow handling procedures that maintain labeled storage conditions. Do not attempt to warm the vial with hot water or microwaves; if room-temperature equilibration is permitted by labeling, it should be done within the allowed time window and with clean handling.
Because injection scheduling is clinician-directed, patients should not transport medication to appointments unless specifically instructed by the care team and the dispensing pharmacy.
Side Effects and Safety
After an intravitreal injection, temporary eye-related symptoms are common. These can include mild discomfort, a gritty sensation, tearing, redness, small conjunctival hemorrhage (a red spot on the white of the eye), transient blurred vision, or floaters. Many symptoms improve over a short period, but patients should follow the post-injection guidance provided by their clinic.
More serious risks are uncommon but important to recognize early. Intravitreal injections can be associated with endophthalmitis (a serious eye infection), retinal detachment, significant intraocular inflammation, or sustained increases in intraocular pressure. Anti-VEGF medicines also carry warnings about possible arterial thromboembolic events (such as stroke or heart attack), although the injection is localized and overall risk assessment depends on individual factors.
Seek urgent eye care if symptoms suggest complications, especially worsening eye pain, increasing redness, marked light sensitivity, a sudden decrease in vision, or increasing floaters over hours to days. Monitoring may include intraocular pressure checks and retinal exams, particularly in patients with glaucoma risk or a history of injection-related complications.
Lucentis Vial is typically used within a safety protocol that emphasizes sterile technique, symptom education, and structured follow-up.
Drug Interactions and Cautions
Because ranibizumab is delivered into the eye, traditional drug–drug interactions are less common than with oral medicines. Even so, clinicians consider the full medication list and medical history when planning intravitreal therapy, especially in patients with recent thromboembolic events or significant cardiovascular risk factors. Tell the ophthalmology team about anticoagulants, antiplatelet therapies, and recent surgeries so the overall risk picture is clear.
Caution is also used when multiple intraocular procedures are planned close together, or when there are active eye conditions that increase complication risk (for example, infection or significant inflammation). If another anti-VEGF agent or intravitreal steroid is being considered, the prescriber will weigh relative labeling, prior response, and tolerability. Pregnancy and breastfeeding considerations should be discussed with the treating clinician, since VEGF inhibition has theoretical fetal risk and individual counseling is needed.
- Report recent eye infection
- List all current medicines
- Discuss cardiovascular history
- Share prior injection reactions
Compare With Alternatives
Several intravitreal therapies are used for similar retinal conditions. Options may include other anti-VEGF medicines such as aflibercept and brolucizumab, as well as steroid-based approaches in selected situations. Choices can depend on the labeled indication, prior response, imaging findings, side effect history, and the clinic’s monitoring strategy.
From a practical standpoint, format can matter. A vial-based workflow may involve additional preparation steps compared with a manufacturer-prepared syringe, and clinics may have preferences based on inventory and procedure-room setup. If your clinician discusses switching presentations, it is usually to streamline clinic processes while maintaining the intended dose and sterile technique.
For on-site comparisons of related products, see Eylea as another anti-VEGF option and Lucentis Prefilled Syringe for an alternative presentation of ranibizumab. Lucentis Vial remains a common single-use format in retina practice, particularly where vial workflows are established.
Pricing and Access
Access to ranibizumab generally requires a valid prescription and coordination with an ophthalmology clinic, since administration is in-office. Coverage rules vary by plan and indication, and many patients encounter utilization management steps such as prior authorization or step therapy. Documentation may include diagnosis details, prior treatment history, and baseline imaging that supports medical necessity.
For patients paying out of pocket, affordability can depend on the prescribed product presentation, site of care, and whether the medicine is billed under pharmacy or medical benefits. If you are evaluating coverage changes or paying without insurance, ask the clinic which billing pathway applies and which documentation they need from your insurer. CanadianInsulin can support referral-style coordination, and dispensing is handled by licensed third-party pharmacies where permitted.
Cross-border fulfilment can be considered in limited cases, and eligibility and jurisdictional rules can affect what is feasible. If an informational page about current programs is relevant, you can review Promotions for general details, keeping in mind that clinical appropriateness and legal requirements come first. For any pathway, accurate prescriber information and matching product identifiers help reduce avoidable delays.
Authoritative Sources
For prescribing indications, warnings, and preparation instructions, refer to the official U.S. label: FDA prescribing information for Lucentis.
For patient-oriented background on retinal disease and anti-VEGF treatment concepts, see: American Academy of Ophthalmology anti-VEGF injections overview.
When medication is supplied through permitted partner channels, handling may involve prompt, express, cold-chain shipping aligned with product requirements and jurisdictional rules.
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is ranibizumab and what does anti-VEGF mean?
Ranibizumab is the active ingredient in Lucentis and is classified as an anti-VEGF medicine. VEGF (vascular endothelial growth factor) is a signaling protein that can contribute to abnormal blood vessel growth and leakage in the retina, which may lead to swelling and vision loss. Anti-VEGF treatments bind VEGF and reduce its activity in the eye. Because ranibizumab is given by intravitreal injection, the intended effect is local to ocular tissues, and follow-up monitoring focuses on vision changes and retinal imaging findings.
How is Lucentis given, and can it be self-injected at home?
Lucentis is administered as an intravitreal injection, meaning the medicine is injected into the vitreous (the gel inside the eye). This is performed by trained ophthalmology professionals using sterile technique in a clinical setting. It is not intended for self-injection at home. The visit may include numbing drops, antiseptic preparation of the ocular surface, and post-injection checks. Your clinic may give instructions about expected short-term symptoms and which signs should prompt urgent evaluation.
What symptoms after an intravitreal injection should be treated as urgent?
After an eye injection, mild irritation, tearing, or a small red spot on the white of the eye can occur. However, certain symptoms can signal complications that need prompt assessment. Contact an eye-care professional urgently for worsening eye pain, increasing redness, marked light sensitivity, a sudden drop in vision, or a rapid increase in floaters. These may be associated with serious issues such as infection (endophthalmitis), retinal detachment, or significant inflammation. Your clinic’s after-hours instructions should specify how to get urgent help.
How often are Lucentis injections given?
The dosing schedule depends on the condition being treated and the prescriber’s plan. For several adult retinal indications, dosing commonly starts with injections at regular intervals (often monthly) and may later be adjusted based on response and monitoring. Some conditions and patient populations can have different dosing approaches, and the label may allow for individualized follow-up strategies. Because timing is tied to exam findings and imaging, clinicians usually set the schedule during follow-up visits rather than using a fixed long-term calendar.
What should I ask my retina specialist before starting ranibizumab?
Helpful questions include: what diagnosis is being treated, what goals are realistic (stabilizing vision vs improving vision), and how response will be monitored (vision testing, OCT imaging). Ask about expected short-term effects after each injection, and what warning signs warrant urgent care. It can also help to discuss your history of glaucoma, recent eye surgery, eye infections, stroke or heart attack, and current blood thinners. If pregnancy or breastfeeding is relevant, request individualized counseling based on risks and alternatives.
What are the key storage requirements for Lucentis vials before use?
Storage should follow the product labeling and pharmacy instructions. In general, Lucentis is kept refrigerated, protected from light, and not frozen. Shaking is avoided because it is a protein-based medicine. Clinics typically keep the product in its original carton until preparation to reduce light exposure and keep identifying information with the medication. If the product is transported between sites, temperature control is important. Patients should not store or transport the medication unless specifically instructed by the dispensing pharmacy and treating clinic.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
Zepbound Side Effects Long-Term: What to Monitor Over Time
Key Takeaways Most effects are gastrointestinal and often improve over time. You may notice symptoms soon after the first injection. Track patterns: timing, triggers, and recovery after each dose. zepbound…
GLP-1 Drugs for Weight Loss: Options, Risks, and Next Steps
Key Takeaways These medicines target appetite signals and digestion to support weight management. Approval and use vary by product, condition, and country-specific labeling. Many options are injections; one GLP-1 medicine…
SGLT2 Inhibitors Mechanism of Action in Heart Failure
Overview Heart failure is not just a “weak heart.” It is a body-wide syndrome that affects fluid balance, kidneys, and energy use. Understanding sglt2 inhibitors mechanism of action in heart…
DPP-4 Inhibitors Weight Loss: What Research Shows Clinically
Key Takeaways DPP-4 inhibitors usually have little effect on body weight. Most studies describe this class as “weight neutral,” not weight-loss therapy. Weight change often depends more on diet, activity,…