Many adults with type 2 diabetes consider using victoza and insulin together. This combination can improve glycemic control when diet and one therapy are not enough. It demands careful monitoring for low blood sugar, gastrointestinal effects, and dose coordination. Use this evidence‑based overview to prepare for a thorough discussion with your clinician.
Key Takeaways
- Combination benefits: May improve A1C and reduce insulin needs.
- Main risks: Hypoglycemia with insulin and gastrointestinal effects.
- Practical points: Rotate injection sites and review sick‑day rules.
- Plan follow‑up: Arrange labs and glucose reviews after changes.
How Victoza Works with Basal and Prandial Insulin
Victoza (liraglutide) is a GLP‑1 receptor agonist that enhances glucose‑dependent insulin secretion and slows gastric emptying. Basal insulin covers fasting needs, while prandial insulin targets meals. Together, these agents can complement each other by addressing different aspects of dysglycemia. Adding a GLP‑1 RA may allow lower mealtime insulin requirements with appropriate oversight.
Patients often ask, is victoza insulin, and the answer is no. It is not insulin; it is an incretin‑based therapy used alongside lifestyle measures. For a broad overview of options and classes, see Common Diabetes Medications for class comparisons and mechanisms. Clinicians typically reassess fasting and post‑meal glucose after any change to align therapy with personal targets.
Regulatory and guideline sources note this pairing may reduce A1C with manageable tolerability. For detailed labeling on indications, risks, and dosing, consult the Victoza prescribing information. For practical sequencing among agents, the ADA Standards of Care 2024 provide framework guidance on GLP‑1 RAs and insulin.
Combining Victoza and Insulin: Safety, Risks, and Monitoring
When these medications are used together, hypoglycemia risk can increase, especially with prandial insulin. Clinicians may consider adjusting meal‑time units when significant appetite suppression occurs. A structured plan for glucose checks—fasting, pre‑meal, and occasional post‑meal—helps identify patterns early. Keep fast‑acting carbohydrates available and review recognition of low blood sugar symptoms.
Gastrointestinal effects, such as nausea and early fullness, may appear during titration. Hydration, smaller meals, and slower dose steps can improve tolerability. Review other hypoglycemia risks, including renal impairment and missed meals. If fixed‑ratio combinations are relevant to your care, see Xultophy Side Effects for combination product risks and what to monitor.
Dosing, Titration, and Injection Sites
Start low and titrate gradually to support tolerability, using clinician‑directed schedules. Do not make dose changes without medical guidance, particularly when insulin is part of the regimen. For step‑by‑step titration and timing considerations, the Victoza Dosing Guide offers detailed, practical instructions to review before clinic visits. Device specifics, including pen features and needle handling, are outlined on the Victoza Pens page for device specifications and proper setup.
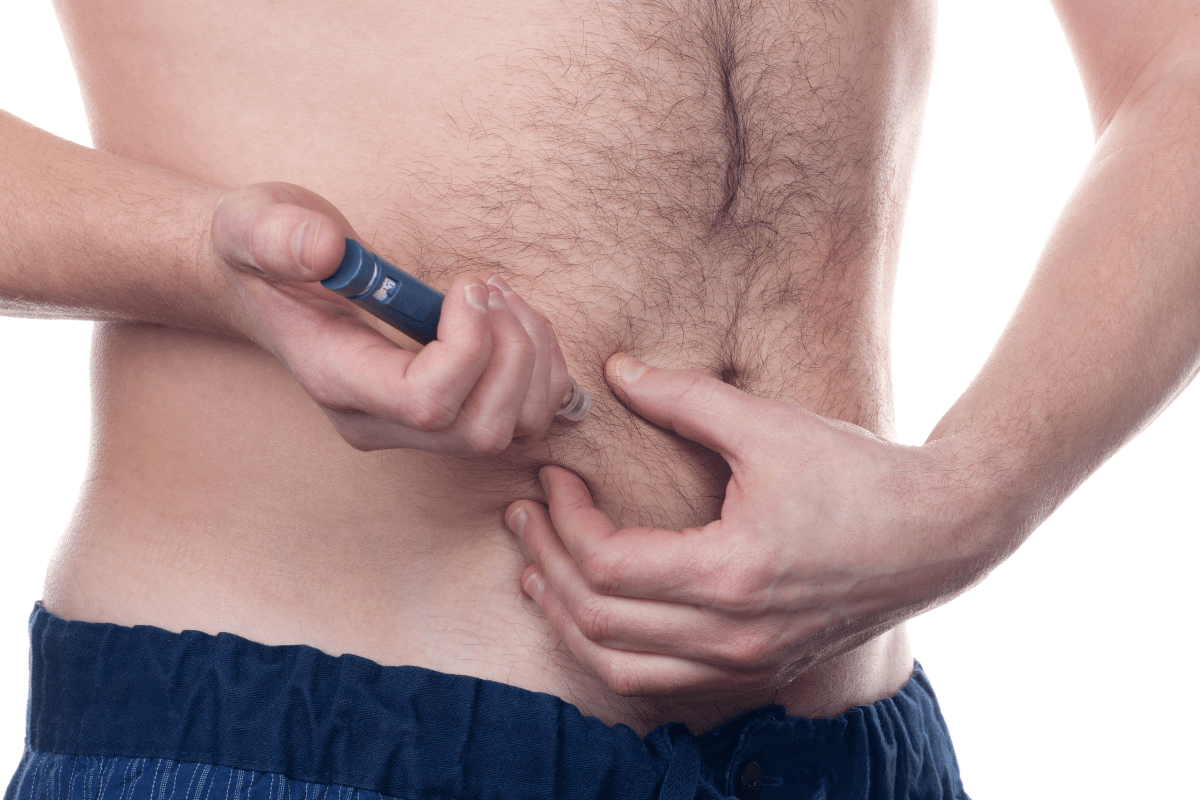
Recommended victoza injection sites include the abdomen, thigh, or upper arm, rotating locations to reduce irritation. Avoid injecting into scar tissue, bruised areas, or sites with lipohypertrophy. Take time to review priming steps, needle disposal, and pen storage temperatures. If you also use mealtime insulin, separate injections by site and technique to prevent confusion and site fatigue.
Weight, Appetite, and Tolerability
GLP‑1 RAs often reduce appetite and support weight management while improving glycemia. When insulin is present, this effect can still occur but requires careful glucose monitoring to limit lows. If nausea limits intake, slow titration and smaller, lower‑fat meals often help. Incorporating gentle activity can further improve post‑meal glucose and comfort.
Common victoza side effects include nausea, diarrhea, decreased appetite, and occasional injection‑site reactions. Report persistent vomiting, signs of dehydration, or severe abdominal pain for timely evaluation. Dietary tweaks may reduce symptoms; for practical food choices and triggers to avoid, see Victoza Foods to Avoid to reduce GI upset during titration. Always coordinate changes with your care team to balance glycemic needs and tolerability.
Comparing GLP‑1 Options and Switching Strategies
Liraglutide is one of several GLP‑1 receptor agonists used with insulin. Formulations differ in dosing frequency, side‑effect profiles, and device usability. For a side‑by‑side look at two common choices, review Victoza vs Ozempic for clinical differences and practical trade‑offs. Alternative agents may suit patients seeking weekly dosing or specific cardiometabolic features.
If your clinician recommends switching from victoza to ozempic, expect a plan that addresses overlap, titration steps, and insulin adjustments. This may include a short washout or timing change to limit additive GI effects. For broader context on GLP‑1 selections, see Trulicity vs Ozempic to understand weekly alternatives, and review Mounjaro Heart Benefits for emerging cardiometabolic data in related incretin therapies.
Practical Use: Storage, Missed Doses, and Expired Pens
Store unopened pens refrigerated within the labeled temperature range, and follow in‑use storage instructions carefully. If you miss a dose, consult the pen guide or your clinician regarding timing; avoid doubling up after prolonged gaps. For insulin users, do not skip meals to compensate for prior day dosing. Keep a written plan to handle travel, illness, and time‑zone changes.
Understand what happens if you use expired victoza: potency and safety cannot be assured, and the product should not be used. Follow disposal guidance and start a replacement pen as directed. For injection hardware coordination, see Insulin Cartridges for device fundamentals and safe handling principles, especially if you also manage separate insulin devices. The official labeling outlines storage thresholds and stability details you can reference.
Costs and Coverage Basics
Coverage and out‑of‑pocket costs vary by plan, geography, and pharmacy benefits. Review your formulary, preferred pharmacies, and any step‑therapy rules before switching or adding therapies. If you are evaluating patient assistance programs, note documentation requirements and refill timelines. For practical budgeting strategies, see Manage the Cost of Victoza for tools and discussion prompts to bring to your insurer.
Medicare beneficiaries often ask about the cost of victoza with medicare because co‑pays can vary across Parts D plans. Formularies may prefer certain GLP‑1 agents or set tier‑based pricing. Ask your pharmacist to run a test claim for your preferred pharmacy. Revisit coverage annually during open enrollment to match evolving benefits.
Patient Resources and Next Steps
Bring your glucose logs, dose history, and symptoms to each appointment. This information helps your clinician adjust therapy while minimizing side effects. Your care plan may also include targets for A1C, time‑in‑range, blood pressure, and lipids. Consider scheduling a pharmacist or educator visit for device training and nutrition review.
People frequently ask how much is victoza with insurance, but the true cost depends on plan design, deductibles, and copay structures. Many plans require prior authorization; documentation of prior therapies can help. For patients exploring oral incretins, Orforglipron vs Rybelsus offers context on tablets in development or use. If you are considering weekly injectables, review dosing calendars to maintain adherence and reduce missed doses.
Recap
Using Victoza with insulin can strengthen glycemic control when coordinated carefully. The pairing may allow lower prandial doses and improved post‑meal numbers, with attention to hypoglycemia and gastrointestinal effects. Focus on measured titration, site rotation, and routine glucose checks. Keep a clear escalation plan, including when to call for advice.
Align therapy choice with personal goals, comorbidities, and coverage realities. Use linked resources to prepare questions for your next visit. Small adjustments—made deliberately—can improve daily control and comfort over time.
Note: The 3 mg daily weight‑management dose belongs to a different liraglutide product, not Victoza. Do not substitute or adjust doses without clinical guidance.
This content is for informational purposes only and is not a substitute for professional medical advice.