Key Takeaways
- Bidirectional link: diabetes may precede or result from pancreatic disease.
- Early signs are subtle; unexplained weight loss with hyperglycemia warrants review.
- Routine population screening is not advised; risk-based evaluation matters.
- Care works best when oncology, endocrinology, and nutrition teams coordinate.
Why the Link Matters
Diabetes and pancreatic cancer intersect in complex, clinically relevant ways. For some adults, new hyperglycemia appears months before a tumor is found. For others, established Type 2 diabetes complicates therapy and recovery. Recognizing patterns early can speed appropriate referrals and monitoring.
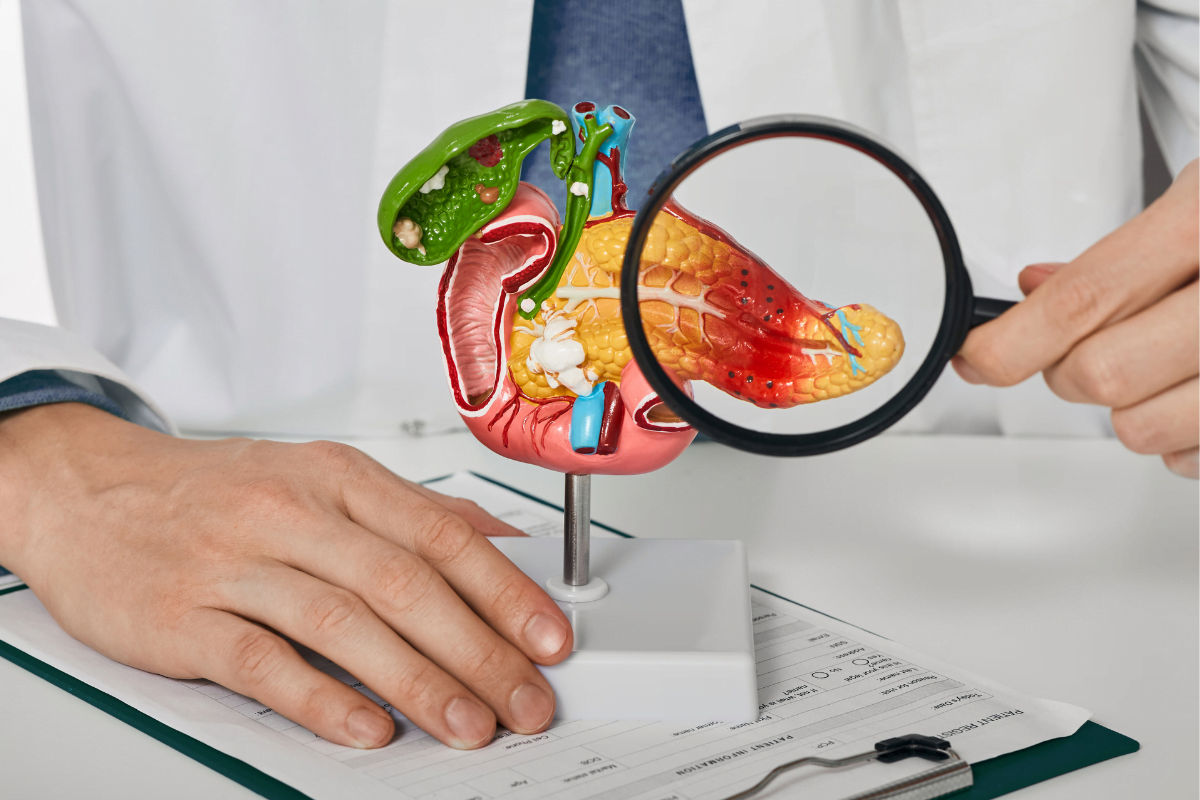
Most people with diabetes will never develop pancreatic tumors, and most tumors occur without diabetes. Still, overlapping metabolic changes, cancer-related inflammation, and pancreatic damage can shift glucose control quickly. For organ-level context, see Link Between Pancreas And Diabetes for a concise overview of endocrine and exocrine roles.
Link Between Pancreas And Diabetes provides foundational anatomy and physiology, which helps interpret glycemic changes during pancreatic illness.
Diabetes and Pancreatic Cancer: What Links Them
Two pathways explain the association. First, tumor-driven factors can induce insulin resistance and impair beta-cell function, producing paraneoplastic dysglycemia (abnormal glucose regulation). Second, pancreatic tissue loss from tumor, surgery, or chronic pancreatitis can reduce insulin and glucagon output, sometimes leading to pancreatogenic diabetes (often called Type 3c).
Mechanisms likely coexist. Cytokines and tumor-derived peptides may worsen hepatic glucose production, while local ductal obstruction triggers fibrosis and exocrine insufficiency. Clinically, patients might show rising glucose, early satiety, and weight loss without obvious infection or steroid exposure. For clarity on pancreatogenic diabetes categories, see Type 3 vs 3c Diabetes to distinguish terminology used in consultations.
Type 3 vs 3c Diabetes outlines features that separate secondary pancreatic diabetes from classic Type 2 presentations.
Early Signs and Symptoms
Early disease often produces vague complaints. People may report appetite change, upper abdominal discomfort, or back pain. Jaundice, dark urine, or pale stools suggest biliary obstruction. Unintentional weight loss with worsening glucose control is a common pattern. These evolving features help frame the differential before imaging.
When discussing surveillance, clinicians usually ask about pancreatic cancer symptoms along with timing, severity, and triggers. Women can show the same early signs as men. However, iron deficiency, fatigue, or subtle digestive changes may be more easily overlooked in busy schedules. Documentation of weight, A1C, and a careful medication history strengthens decision-making and referral.
Broader risk context is helpful; the article Diabetes Risk Factors summarizes metabolic, genetic, and lifestyle contributors that may overlap with pancreatic disease.
Diabetes Risk Factors offers a practical checklist to review during intake assessments.
Does Cancer Trigger Diabetes?
Evidence supports a bidirectional association, but the temporal pattern is key. The question does pancreatic cancer cause diabetes is best answered with nuance: in some adults, tumor biology appears to precipitate insulin resistance and impaired insulin secretion, creating new-onset hyperglycemia. In others, long-standing diabetes increases cancer risk modestly.
Not every case of new diabetes signals malignancy. Age over 50, rapid weight loss, low body mass index, or abrupt insulin requirement increases the index of suspicion. The American Cancer Society notes a higher prevalence of diabetes among people with this malignancy, underscoring vigilance without overtesting. For high-level background from an authoritative source, see the American Cancer Society overview (American Cancer Society).
Glucose Patterns, A1C, and Monitoring
Several glycemic patterns raise attention. Some patients develop fasting hyperglycemia (high blood sugar) with normal postprandials. Others have swings related to malabsorption and reduced pancreatic enzymes. Monitoring trends, not single readings, helps detect meaningful change without undue alarm and guides follow-up planning.
Clinicians may note a rising pancreatic cancer a1c despite stable diet, activity, and medications. Concurrent weight loss or steatorrhea suggests exocrine issues. Capillary monitoring can be reinforced with connected meters to capture variability. For practical device guidance, see Freestyle Freedom Lite Meter for everyday tracking steps, and consider OneTouch Verio Flex Meter when Bluetooth summaries support remote review.
Freestyle Freedom Lite Meter explains setup and thresholds that aid pattern recognition in primary care.
OneTouch Verio Flex Meter can help patients share trends during oncology or endocrinology visits.
Screening and Referral Triggers
Population-wide screening for this tumor is not recommended in asymptomatic adults. The USPSTF recommendation advises against routine screening due to low incidence and potential harms. Instead, targeted evaluation is suggested for people with concerning constellations such as new-onset diabetes pancreatic cancer pattern with weight loss, abdominal pain, or jaundice.
Reasonable steps include focused examination, medication review, and appropriate imaging if red flags persist. Some clinicians assess tumor markers in select contexts, though these are not screening tests. The USPSTF statement provides useful perspective on when testing helps or harms; see their guidance (USPSTF recommendation). Exocrine disorders also matter; Pancreatitis and Diabetes highlights how inflammation and scarring can change glycemic control and mimic malignancy features.
Pancreatitis and Diabetes discusses preservation strategies that inform differential diagnosis and follow-up.
Treatment and Multidisciplinary Care
Coordination across oncology, endocrinology, surgery, and nutrition improves safety and outcomes. Glycemic targets may need individualization during chemotherapy, radiation, or post-operative recovery. Insulin is often used because of variable intake and organ stress, while non-insulin agents may be considered case-by-case with attention to side effects and renal function.
Plans for pancreatic cancer and diabetes treatment balance tumor control with safe glucose management. Metformin remains a first-line agent for many with adequate renal function, and research continues on its antineoplastic potential. For background on emerging science, see Metformin’s Anti‑Cancer Properties for mechanisms under study. Complex regimens sometimes require combination therapy; Diabetes Medication Combinations summarizes common pairings that clinicians review when adjusting care.
Metformin’s Anti‑Cancer Properties explores laboratory and clinical signals relevant to oncology discussions.
Diabetes Medication Combinations provides a structured view of agents often used in complex cases.
Nutrition and Daily Management
Nutrition therapy supports weight, symptom control, and glycemia. Small, frequent meals with adequate protein can reduce postprandial swings. If exocrine insufficiency is suspected, clinicians may assess for pancreatic enzyme replacement therapy (PERT) to improve nutrient absorption. Hydration and fiber choices are adjusted for comfort and tolerance.
A practical diet for pancreatic cancer and diabetes emphasizes energy-dense foods, modest carbohydrate loads, and timing that matches medication action. Home monitoring informs dose adjustments and prevents hypoglycemia during reduced intake days. Proper injection technique also matters when insulin is used; BD Nano Pro Pen Needles can improve comfort, which encourages consistent dosing. For broader reading, browse Diabetes Articles for self-management guides across common scenarios.
BD Nano Pro Pen Needles may support adherence by reducing discomfort during frequent injections.
Diabetes Articles collect practical guides that patients and caregivers can reference.
Related Topics and Further Reading
Adjunct issues can influence presentation and care. For instance, GLP‑1 receptor agonists have been discussed in the context of pancreatitis risk; the article Wegovy and Pancreatitis reviews signals and precautions. Understanding inflammatory pathways helps clinicians interpret abdominal symptoms and laboratory changes during metabolic treatment.
Oncology content evolves quickly. To track developments, browse Cancer Articles for background primers and updates on terminology, staging, and supportive care. Clinicians planning regimen reviews can also survey Cancer Medications for a high-level view of agents commonly encountered during multidisciplinary coordination.
Wegovy and Pancreatitis discusses safety considerations that sometimes intersect with abdominal complaints.
Cancer Articles consolidate foundational reading on tumor biology and supportive care planning.
Cancer Medications provides category-level context useful during reconciliation and counseling.
Recap
The link between metabolic disease and pancreatic malignancy is real but nuanced. Most people with diabetes will not develop this cancer, yet abrupt glycemic shifts with systemic symptoms merit attention. Risk-based evaluation, careful monitoring, and coordinated care improve safety without overtesting.
When uncertainty remains, clinicians can combine history, examination, and targeted imaging rather than defaulting to broad screening. Current recommendations discourage population screening, but they support timely workup of red flags. For epidemiology and patient-focused overviews, the National Cancer Institute maintains accessible summaries and updates (National Cancer Institute).
Note: Document baseline weight, medications, and glucose trends to detect meaningful change early.
This content is for informational purposes only and is not a substitute for professional medical advice.