Understanding lantus insulin injection sites helps you inject consistently and comfortably. Good site selection and rotation lower the chance of lumps and variability in absorption. This guide explains where to inject, how to rotate, and practical pen techniques.
Key Takeaways
- Preferred areas: abdomen, thigh, upper arm, and upper buttock.
- Rotate within and between regions to prevent tissue changes.
- Keep technique consistent: depth, angle, dwell time, and needle size.
- Store pens correctly and track opened dates to protect potency.
- Watch for lipohypertrophy (fatty lumps) and avoid affected spots.
What Lantus Is and Why Sites Matter
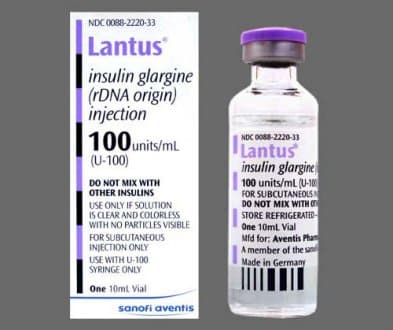
Lantus (insulin glargine) is a long-acting basal insulin that releases slowly. The goal is steady background coverage, not rapid corrections. Tissue thickness and local blood flow can influence onset and predictability. Incorrect depth, scar tissue, or repeated use of one spot may cause erratic absorption.
People often ask how much does lantus lower blood sugar. The effect varies by dose, timing, site, and individual sensitivity. Keeping your method consistent helps reduce day-to-day swings. Site rotation is a simple lever you control, alongside meal planning and monitoring.
For device handling basics, see Lantus Insulin Pen for step-by-step context. If you use vials and syringes, the Lantus Vial Stability overview explains vial-specific handling.
Lantus Insulin Injection Sites: Where and Why
Preferred subcutaneous regions include the abdomen (away from the navel), front or outer thigh, back of the upper arm, and upper outer buttock/hip. These areas typically offer consistent fat depth for subcutaneous delivery. Avoid scars, moles, bruises, hardened areas, and sites with infection or visible inflammation. Give at least two inches of space from the belly button when using the abdomen.
Rotation matters because repeated injections into one spot may lead to lipohypertrophy (fatty tissue build-up) or lipoatrophy (fat loss). These changes can blunt or accelerate insulin uptake and increase discomfort. A simple quadrant or grid system helps: pick a region for the week, move the injection point at least one inch each time, and switch regions weekly. Record sites in a log to prevent drifting back to the same point.
Abdomen, Thigh, Arm, Buttock: Pros and Cons
The abdomen often provides the most consistent absorption for basal insulin. Thighs and upper buttocks are convenient for self-injection and offer adequate fat depth in many adults. Upper arms can be used, but some people require assistance to reach the correct back area safely. If your skinfold is thin, consider shorter needles and a lifted skinfold to keep injections subcutaneous.
Discomfort can vary by location and needle length. If an area becomes tender or bruised, switch to a different region until it resolves. Do not inject into areas with numbness or significant scarring, since feedback and absorption can be unreliable.
Manufacturer guidance on subcutaneous use and site rotation is summarized in the Lantus prescribing information, which outlines approved regions and technique basics.
Rotation Strategy and Site Assessment
Use a structured plan so you do not guess each day. For example, divide the abdomen into four quadrants and move clockwise across small, non-overlapping points. Next week, switch to the thigh and repeat a similar pattern. Consistent spacing helps limit tissue stress and keeps absorption similar from one dose to the next.
Before injecting, palpate the area gently. Feel for rubbery thickened spots, nodules, or depressions. If you notice changes, skip that area for several months and document the finding. Ask your clinician to examine suspected lipohypertrophy at your next appointment. When selecting Insulin Pen Needles Guide, review size options and bevels to match your skinfold; this supports consistent depth and comfort.
Many clinics teach rotation using simple diagrams. If you prefer visual learning, NIDDK provides practical injection guidance; see the NIDDK injection instructions for safe technique fundamentals.
Technique With Pen Devices
Prepare your pen by checking the label, inspecting the insulin, and attaching a new needle. Prime per device instructions until a steady drop appears. Select the dose, clean the skin if desired, and inject at 90 degrees in most adults. Press and hold the button for 10–15 seconds to allow full delivery, then remove the needle straight out.
If your skinfold is thin, lift a gentle pinch to avoid intramuscular placement. Typical modern pen needles are 4–6 mm; longer options may suit higher skinfolds. Do not reuse needles, since reused tips can bend and tear skin. For device orientation and daily use scenarios, see Lantus Insulin Pen for device-specific nuances and troubleshooting.
Beginners often ask about videos and printable steps. While formats vary, the core actions are consistent across brands. Training from your care team stays essential, even if you watch tutorials. The pen platform you use can influence small steps like priming, so follow your device’s manual for precision.
Some patients refer to a lantus insulin pen for their daily basal dose. Keep pen angle, depth, and dwell time the same each day to support steady absorption.
Dose Timing, Missed Doses, and Safety Checks
Basal insulin works best when taken at the same time each day. Many adults pick evening hours, but timing should remain consistent. If you miss a dose, follow your clinician’s plan; do not double up without guidance. Use caution with correction doses from rapid-acting insulin if your basal timing has shifted.
Signs of localized problems include persistent pain, redness, warmth, or thickened skin. Unexplained glucose variability can also signal site issues. Document the region, depth, and time of day when unusual readings appear. Talk with a clinician about when to not take lantus, including during episodes of recurrent hypoglycemia or when directed to pause around certain procedures.
For a broader discussion of adverse effects and what to monitor, see Lantus Side Effects for context on symptom patterns and next steps.
Storage, Pen Counts, and Cartridge Details
Unopened pens should be refrigerated per label, and opened pens kept at room temperature within the specified time window. Track the date you first used each pen and discard on schedule. Avoid heat, freezing, and direct sunlight. If insulin looks cloudy, colored, or contains particles when it should be clear, do not use it.
Packaging questions are common, including how many lantus pens in a box. Pen counts and volumes vary by market, but SoloStar commonly supplies multiple pens per pack, each typically 3 mL at U-100 strength. Needles are usually sold separately; check your packaging and local standards. For specifications on the device you use, the Lantus SoloStar Pens product page provides size and format details for planning refills.
If you prefer cartridges and compatible reusable pens, review the Lantus Cartridge Guide for handling and safety tips. For biosimilar alternatives and supply logistics, see the Basaglar Cartridge article, which outlines similarities and device considerations.
For storage thresholds and stability statements, the official prescribing information summarizes labeled temperature limits and in-use periods.
Related Basal Options and Comparisons
Concentration and delivery differences can affect dose volume and absorption. Understanding these nuances helps you interpret glucose trends rather than chasing daily noise. Discuss alternatives when steady-state patterns are hard to achieve despite consistent technique and rotation.
When comparing long-acting insulins, consider pharmacology, pen design, and titration guidance. Many adults ask about the difference between lantus and toujeo. Toujeo is a more concentrated insulin glargine formulation, and clinical teams may use it when volume considerations matter. For a broader lens on product profiles, review Tresiba vs. Lantus as a structured comparison, and see Toujeo Overview for concentration-specific details.
Safety at the Injection Site
Lipohypertrophy presents as rubbery, painless lumps that can delay or blunt insulin action. Regularly inspect and palpate sites under good lighting. If you detect changes, mark the area on a rotation chart and avoid it for several months. Consider shorter needles or a lifted skinfold if you frequently encounter bruising or pain.
People sometimes wonder: will lantus lower blood sugar quickly. As a basal insulin, its effect is designed to be gradual. If you notice rapid drops after an injection, check for confounders like unexpected exercise, meal mismatch, or unintentional intramuscular delivery. Review needle length, angle, and pinch technique to maintain subcutaneous placement. For side effect patterns beyond the skin, see Insulin Side Effects to understand broader risks and mitigation.
Tip: Keep a simple rotation map on your phone or logbook. A quick glance before each dose helps maintain spacing and consistency.
Recap
Site selection and rotation are quiet levers that keep basal insulin predictable. Use structured patterns, consistent technique, and regular skin checks to avoid tissue changes. Align device handling with label guidance and your clinician’s plan. For deeper reading, browse Diabetes Articles covering devices, storage, and comparative options.
This content is for informational purposes only and is not a substitute for professional medical advice.