Insulin Glargine is a long-acting basal insulin designed to provide steady background control. This guide explains timing, how it behaves in the body, and practical use. You will also find device handling, storage, and safety fundamentals.
Key Takeaways
- Flat action profile: minimal peak and roughly 24-hour coverage.
- Timing matters: dose consistently at the same time each day.
- Device handling: pens, vials, and cartridges require correct technique.
- Safety first: watch for low glucose and known interaction risks.
Insulin Glargine: Onset, Peak, and Duration
Glargine is classified as a long-acting basal insulin (background insulin). After subcutaneous administration, the onset typically occurs within a few hours. It forms microprecipitates in the subcutaneous tissue, which dissolve slowly and release insulin at a near-constant rate. This slow release helps reduce glycemic variability (blood sugar swings) across the day and night.
Most people experience a near-flat profile with no pronounced peak. Duration commonly approaches 24 hours, though some may need twice-daily dosing for full coverage. Temperature, injection site, and individual pharmacokinetics (how the drug moves in the body) can shift both onset and duration. For label-supported details on timing and profile, see the Sanofi U.S. prescribing information for Lantus prescribing information.
Factors That Shift Timing
Absorption can vary based on injection site, depth, and local blood flow. Warmer skin or light exercise near the injection time may slightly speed uptake. Lipohypertrophy (thickened fatty tissue) from repeated injections in the same spot can slow and make absorption unpredictable. Rotating sites within the same region helps consistency over weeks. Body weight, renal function, and concurrent medications also influence timing. When patterns change, review technique, sites, and timing before adjusting any regimen.
How It Works in the Body
At the molecular level, glargine is modified human insulin. After injection, it precipitates in subcutaneous tissue and gradually redissolves. The released insulin binds insulin receptors to facilitate glucose uptake and suppress hepatic glucose output. This basal effect complements mealtime insulin by covering fasting and between-meal needs.
Clinically, the formulation’s steady kinetics aim to reduce nocturnal hypoglycemia and fasting variability. The flatter profile contrasts with intermediate-acting preparations that show more pronounced peaks. For additional background on insulin action in daily life, see How Lantus Works for device behavior and pharmacology context.
As a concise term pairing science and practice, insulin glargine mechanism of action describes this slow release from microprecipitates and stable receptor engagement over many hours.
Dosing Fundamentals and Titration
Dosing is individualized and should be supervised by a clinician. Typical titration aims to reach fasting targets without excessive lows. Small, scheduled adjustments at regular intervals are common strategies. Many patients take their dose at night for convenience, but morning dosing can also be effective when aligned with daily routines.
Patients often ask how many units of lantus is normal. The answer varies by body weight, age, concurrent therapies, and clinical goals. Consistent timing supports stable fasting values; this is why plans may emphasize lantus dosing at bedtime for some users. For broader context on titration frameworks and alternatives, see Basal Insulin Types for methods used in practice.
Pen Devices and Handling
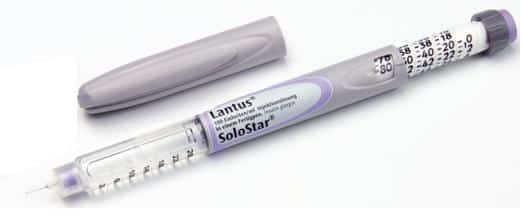
Delivery devices include disposable pens, reusable pens with cartridges, and multidose vials. Each option requires correct priming, dialing, and injection technique. The Lantus SoloStar Insulin Pen article offers device steps and troubleshooting guidance. Many patients favor pens for convenience, dose accuracy, and reduced need for supplies.
Users frequently mention lantus solostar when discussing ease of use during travel or busy schedules. If you and your clinician select a disposable pen, you can review specifications in Lantus Solostar Pens 100 Units Ml for presentation details. If vials are preferred for syringe dosing or split regimens, see Lantus Vial 100 Units Ml for format and concentrations.
Storage and Stability
Cold-chain handling preserves insulin potency from the pharmacy to your refrigerator. In-use pens and vials are typically kept at room temperature within stated time limits to reduce injection discomfort; unopened stock remains refrigerated. For specific handling windows and temperature limits, consult the manufacturer’s labeled instructions. The practical steps are straightforward but must be consistent week to week.
Check pens and vials for clarity and expiration before every injection. Avoid freezing, direct heat, or prolonged sunlight exposure, since these conditions degrade potency. For common pitfalls and storage thresholds across formats, see Lantus Vial Guide covering stability cues and disposal timing. Clear routines around lantus insulin storage can help maintain dose predictability and reduce glucose swings.
Safety, Contraindications, and Interactions
Hypoglycemia remains the most important risk with any insulin therapy. Learn the signs of low glucose and keep a plan for rapid carbohydrate on hand. Dosing errors, skipped meals, or unplanned activity can precipitate lows. Alcohol use also increases the risk. Certain comorbidities may require closer monitoring.
Clinicians assess insulin glargine contraindications with a patient’s full history in mind. Be cautious with drugs that alter insulin sensitivity or mask hypoglycemia symptoms, including non-selective beta-blockers. Sulfonylureas and prandial insulin can compound low-glucose risk. For guideline-style safety context and treatment standards, the American Diabetes Association provides annual practice guidance; see the ADA Standards of Care overview standards of care for broad principles.
Comparing Basal Options
Some regimens switch between glargine and other long-acting insulins to meet lifestyle or coverage needs. Differences include duration, peak profile, and pen design. For head-to-head discussion of two leading options, see Tresiba vs Lantus for duration and variability themes. A second comparison outlines legacy and modern patterns; consult Levemir vs Lantus Guide for switching considerations.
Higher-strength glargine and degludec can provide longer windows in specific cases. To explore options and decision points, see Degludec vs Glargine for duration and dosing intervals. If your clinician recommends a concentrated glargine, review its profile in What Is Toujeo for concentration-related differences. Device selection may also matter in practice, and you can check presentation details for concentrated pens in Toujeo Doublestar Prefilled Pen when evaluating format and capacity.
Populations and Indications
Basal therapy supports both type 1 diabetes and type 2 diabetes when indicated by individual goals. In type 1 diabetes, basal is paired with mealtime insulin for complete coverage. In type 2 diabetes, basal may be added when oral agents no longer control fasting values. Plans should account for age, renal function, hypoglycemia risk, and comorbidities.
Pregnancy and breastfeeding require tailored management. Clinicians may consider alternative regimens or closer monitoring during each trimester. For counseling considerations before and during pregnancy, see Lantus in Pregnancy for risk–benefit framing. When insulin therapy relates to weight changes, you can review contributing factors in Lantus and Weight Gain for lifestyle and medication context. For label-defined uses and safety updates, consult the manufacturer’s document prescribing information.
Nursing Considerations and Education
Clinical teaching emphasizes consistent timing, correct injection technique, and hypoglycemia prevention. Demonstrate device priming, dose dialing, and site rotation methods. Review recognition and treatment of mild, moderate, and severe hypoglycemia. Discuss driving safety and how illness or steroids may alter insulin needs. Encourage glucose logging that notes timing, meals, and activity to guide adjustments.
Standard education also covers sick-day rules and when to call for help. Patients should know to avoid mixing long-acting products in the same syringe and to verify dose units before administration. Teaching plans often include reminders about room-temperature storage while in use and refrigeration for unopened supplies. Documentation of teaching and return demonstration supports quality and safety. For clinician-facing summaries, insulin glargine nursing considerations highlight these practical checkpoints during follow-up visits.
Patient Education Points
Use the same time daily and set reminders for adherence. Rotate sites within one region to avoid lipohypertrophy and absorption variability. Keep fast-acting glucose available to treat lows, especially after exercise or alcohol. Record unusual readings, symptoms, or missed doses in a log to share with your clinician. Review expiration dates monthly to prevent underdosing from degraded insulin. Read the device’s manual and perform a brief prime before each injection to confirm flow.
Tip: If your regimen changes or you add mealtime insulin, revisit technique and timing. For step-by-step device guidance, return to the Lantus SoloStar Insulin Pen resource for priming specifics and dose confirmation steps.
This content is for informational purposes only and is not a substitute for professional medical advice.