Overview
Many people hear about “incretin” medicines and want a clear explanation. This article explains what’s behind the mounjaro vs ozempic mechanism of action in plain language. You’ll learn how these drugs interact with gastrointestinal hormones, the pancreas, and the brain. That context helps you compare benefits, side effects, and follow-up needs with your clinician.
Both medicines act on incretins, which are hormones released after you eat. Incretins help your body coordinate insulin release, slow digestion, and change hunger signals. The two drugs are different, though. One is a GLP-1 receptor agonist (a GLP-1 “mimic”). The other is a dual GIP/GLP-1 agonist (it targets two incretin receptors). If you want deeper comparisons beyond biology, see Tirzepatide vs Semaglutide.
Why it matters: Mechanism details often explain why side effects cluster in the gut.
CanadianInsulin is a prescription referral platform, not a dispensing pharmacy.
Key Takeaways
- mounjaro vs ozempic mechanism of action differs by receptor targets.
- Both influence insulin release and glucagon signaling after meals.
- Slower stomach emptying can affect fullness and nausea risk.
- Brain pathways also shape appetite and food cravings.
- Mechanism does not replace individualized prescribing decisions.
Mounjaro vs Ozempic Mechanism of Action: What Happens in the Body
At a high level, these medicines “extend” natural meal-time hormone signals. They amplify incretin messages that normally rise after eating and fade quickly. With medication, that signaling lasts longer, which can change glucose control, digestion speed, and appetite regulation. The details matter because one drug acts mainly through the GLP-1 receptor, while the other engages both GLP-1 and GIP receptors.
Mechanism is not just a single switch. The effects come from a chain of signals across organs. The gastrointestinal tract releases incretins, the pancreas adjusts insulin and glucagon output, and the stomach may empty more slowly. Meanwhile, brain circuits that regulate satiety (feeling full) receive different “stop eating” cues. Your outcomes and side effects can vary based on diet patterns, other medications, and underlying conditions.
Core Concepts
Before comparing brands, it helps to map the shared biology. The mounjaro vs ozempic mechanism of action sits inside the incretin system, which is part endocrine and part neurological. Think of it as coordinated messaging between the gut, pancreas, liver, stomach, and hypothalamus (a brain region that helps regulate hunger).
In real life, these pathways overlap. A single change, like slower digestion, can also affect glucose peaks and hunger timing. That is why clinicians often watch both lab results (like A1C) and day-to-day tolerance.
Incretin Hormones Explained
Incretins are hormones released from your gastrointestinal tract when nutrients arrive. Two key incretins are GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). They help coordinate “after-meal” metabolism. In simple terms, they tell the pancreas when to increase insulin, and they influence how much glucagon is released. Glucagon is a hormone that signals the liver to release stored glucose.
Incretins also interact with the nervous system. GLP-1 signaling is linked to satiety or the feeling of fullness and reduced appetite in many people. These effects involve central appetite regulation, including hypothalamic circuits such as the POMC pathway (a satiety-promoting neuron network). The takeaway is that incretins are not just “blood sugar hormones.” They affect eating behavior, digestion timing, and hormone balance.
GLP-1 Receptor Agonist Mechanism
GLP-1 receptor agonists mimic the body’s GLP-1 signal. Their effects are often described through three main levers. First, they support glucose-dependent insulin secretion, meaning insulin release tends to increase when glucose is higher. Second, they reduce glucagon output in a glucose-dependent way, which can lower the liver’s glucose release after meals. Third, they slow gastric emptying (stomach emptying), which can blunt post-meal glucose spikes and increase fullness.
They also act through the brain. GLP-1 receptors in the central nervous system are part of energy balance and satiety signaling. This includes appetite suppression mechanisms that can change cravings and portion sizes. Because the digestive tract is directly affected, nausea and other GI symptoms are understood as “on-target” effects for some people, especially during dose escalation phases. For a class-level comparison, see Trulicity vs Ozempic.
GLP-1 vs GIP Mechanism
GIP is another incretin with different biology. Like GLP-1, GIP can enhance insulin secretion when glucose is elevated. Its effects are context-dependent, and its receptor is expressed in several tissues. Researchers study GIP for potential roles in nutrient handling, fat tissue signaling, and how the body partitions energy after meals. In practice, “dual agonism” aims to integrate these signals rather than relying on GLP-1 alone.
Clinically, people often summarize this as “two pathways instead of one,” but the reality is more nuanced. Receptor activation depends on pharmacodynamics (what the drug does to the body), receptor affinity (how strongly a drug binds), and downstream signaling bias (which internal cell pathways are activated). Those differences may help explain why people can respond differently to two incretin-based drugs, even when both are used for similar metabolic goals.
Tirzepatide Pharmacodynamics Overview
Tirzepatide is designed as a dual GIP/GLP-1 receptor agonist. That means it activates two incretin receptors that influence insulin secretion, glucagon suppression, and appetite regulation. “Dual” does not mean “twice as strong.” It means the drug engages two receptor families with different distribution and signaling patterns. Because of that, clinicians often consider both glucose metrics and tolerability, not just one endpoint.
Incretin activity can support beta cell function (the insulin-producing cells of the pancreas) indirectly by reducing glucose stress over time. However, individual biology matters. Diet composition, baseline insulin resistance, and other medications can shift how the incretin system behaves. Dose-response concepts also matter: a stronger receptor signal can increase desired metabolic effects, but it can also amplify GI side effects for some people.
Semaglutide Pharmacodynamics Overview
Semaglutide is a GLP-1 receptor agonist. Its pharmacodynamic profile centers on GLP-1 receptor activation across the pancreas, gut, and brain. In the pancreas, semaglutide supports glucose-dependent insulin secretion and reduces inappropriate glucagon release. In the gut, delayed gastric emptying can contribute to smaller post-meal glucose excursions. In the brain, it can influence satiety and reward pathways tied to eating behavior.
Semaglutide also has evidence-based cardiovascular labeling in specific populations, depending on the product and indication. That distinction is part of “mechanism in context.” A drug’s real-world role is shaped by both biology and labeling, including who it is approved for and what outcomes were studied. For another semaglutide-based comparison, see Victoza vs Ozempic.
Nausea and GI Side Effects Mechanism
GI side effects are common discussion points with incretin-based therapies. A leading explanation is slowed gastric emptying and altered gut-brain signaling. When the stomach empties more slowly, you may feel full sooner or for longer. That can be helpful for satiety, but it can also trigger nausea, bloating, reflux symptoms, or constipation in some people.
There may also be direct central effects. GLP-1 pathways in the brainstem and hypothalamus can affect nausea and food aversion. In addition, changes in bile flow and gallbladder motility have been discussed in clinical literature for the GLP-1 class. This is one reason clinicians take abdominal symptoms seriously, especially if pain is persistent or severe. Mechanism discussions are useful, but they never replace symptom-based evaluation.
Practical Guidance
If you are comparing incretin-based options, focus on a few concrete questions. Start with the approved indication for your situation, then discuss monitoring and tolerability. Bring a list of other medications, especially those that affect blood glucose or digestion. Ask how to recognize common side effects versus symptoms that need prompt clinical review. If you are using a semaglutide product, note that formulations differ, including an oral option; see Rybelsus Semaglutide Pills as an example of a non-injectable formulation.
Quick tip: Keep a simple weekly log of GI symptoms and meal timing.
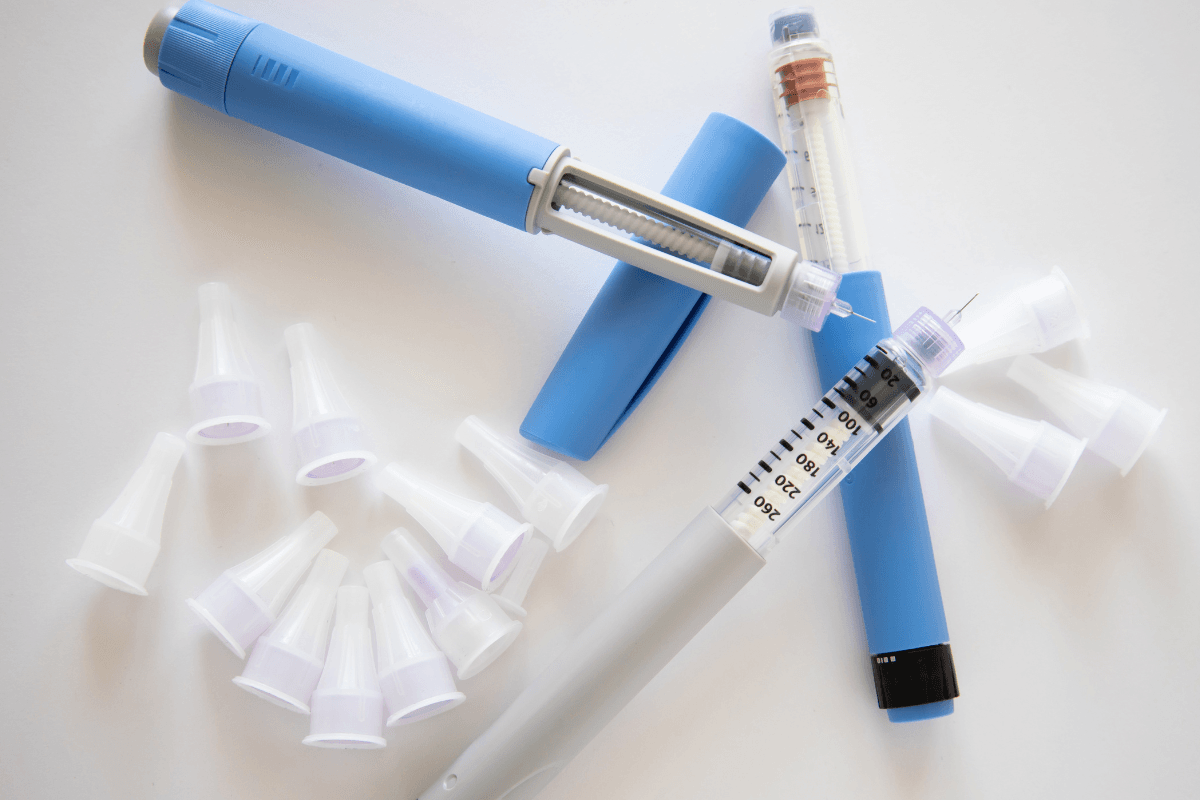
For people reviewing the mounjaro vs ozempic mechanism of action as part of a treatment conversation, it helps to separate “how it works” from “how it’s used.” Mechanism is about receptors and pathways. Use is about dosing schedules, titration plans, contraindications, and follow-up labs, which only your prescriber can individualize. If you need a reference point for the specific products discussed in your visit, you can review Mounjaro and Ozempic Semaglutide Pens for basic identification details.
When needed, prescriptions are confirmed with your prescriber before dispensing.
If switching is part of the discussion, avoid assuming a direct one-to-one equivalence. Even within incretin therapies, differences in receptor targeting, side-effect patterns, and device formats can change the transition plan. People also vary in sensitivity to delayed gastric emptying, which affects nausea risk and food tolerance. Your clinician may also consider comorbidities such as kidney disease, prior pancreatitis history, or gallbladder disease, since these can influence risk discussions and monitoring choices.
Compare & Related Topics
Mechanism comparisons are often most useful when tied to a real decision. For example, you might be weighing a GLP-1-only approach versus a dual incretin approach, or comparing injectable versus oral administration. You may also be looking at different approved indications across related products. For broader context on weight-management labeling differences, see Wegovy vs Mounjaro and Zepbound vs Mounjaro.
It also helps to recognize what mechanism cannot tell you. The mounjaro vs ozempic mechanism of action does not specify which medicine is “better” for a given person. It does not account for insurance rules, supply constraints, or your prior response to similar drugs. It also cannot predict who will develop troublesome nausea. Those are individual factors, best addressed through follow-up and symptom tracking.
| Mechanism area | What it can influence | Why it shows up clinically |
|---|---|---|
| Pancreas (beta cells) | Glucose-dependent insulin secretion | Lower post-meal glucose in some people |
| Alpha cells / liver signaling | Glucagon suppression | Reduced hepatic glucose output after meals |
| Stomach and intestines | Gastric emptying delay | Fullness and GI tolerability patterns |
| Brain appetite circuits | Central satiety signaling | Changes in hunger and cravings |
Several newer and emerging therapies are also built around incretin biology, including oral non-peptide options and multi-agonists. If you want to understand where the field is heading, read Orforglipron vs Tirzepatide. For a broader browsing view of additional explainers, you can use the Articles Archive.
Access topics sometimes come up alongside clinical questions. Some people use cash-pay options, including those without insurance, when coverage is limited. CanadianInsulin supports cross-border access models such as US delivery from Canada, while still requiring a valid prescription.
Authoritative Sources
For the most reliable details, use official prescribing information and regulator-reviewed labeling. These documents define indications, contraindications, warnings, and clinically studied outcomes. They also describe adverse reactions and medication interactions in standardized language.
Here are two primary sources to consult alongside your clinician:
Medications are dispensed by licensed Canadian pharmacies for cash-pay access, often without insurance.
Mechanism is a helpful lens for informed conversations. It clarifies why these drugs can affect blood sugar, appetite, and the GI tract. For next steps, bring your questions to a licensed clinician and review the official label for your specific product.
This content is for informational purposes only and is not a substitute for professional medical advice.
________________________________________________________________________________________________________
Medically Reviewed By: Ma Lalaine Cheng.,MD.,MPH