Reports linking semaglutide and vision changes remain uncommon, but they matter. Most people tolerate GLP-1 therapies well. Still, a small subset may notice visual symptoms during treatment or after rapid glucose improvements. This article clarifies potential mechanisms, outlines monitoring steps, and highlights who may need closer follow-up.
We focus on eye-health basics that support safer use of GLP-1 and GLP-1/GIP medicines. You will see how to prepare for ophthalmology visits, what symptoms deserve urgent attention, and when to seek earlier review. We also summarize practical ways to document changes while treatment continues.
Key Takeaways
- Early eye review: Baseline and follow-up dilated exams help detect changes.
- Watch symptoms: New floaters, eye pain, or sudden vision loss need urgent care.
- Known risks: Rapid A1C improvement can temporarily blur vision in diabetes.
- Targeted follow-up: Retinopathy or vascular risk factors warrant closer monitoring.
What Recent Studies Show
Observational signals have raised questions about rare optic nerve events during GLP-1 therapy. Some patients on these agents reported sudden vision changes or optic neuropathies. These events remain uncommon, and causation is not established. Clinicians should balance the benefits of cardiometabolic control against small, uncertain ocular risks while maintaining routine screening.
Case series and cohort analyses have discussed potential links to ischemic optic neuropathy, prompting more research. Public discussions sometimes frame these concerns as semaglutide blindness, which overstates the evidence. For background on nonarteritic anterior ischemic optic neuropathy (NAION), the American Academy of Ophthalmology provides a concise overview that explains presentation and risk factors (AAO NAION overview). Until stronger data arrive, the practical approach remains steady: routine ophthalmic care and prompt evaluation of new symptoms.
If you want broader context on diabetes and eye care, our Ophthalmology coverage collects relevant topics and screening guidance for ongoing reference.
How Could These Drugs Affect the Eyes?
GLP-1 therapies can accelerate glucose improvement, and quick shifts in blood sugar can temporarily alter the eye’s lens shape. This may cause short-lived blur or shifting prescriptions. Dehydration, changes in blood pressure, or vascular tone could also affect retinal and optic nerve perfusion. These mechanisms are plausible, but the magnitude of risk appears low for most users.
In product labeling, diabetic retinopathy complications are noted, particularly when glucose control improves rapidly. Patients with established retinopathy may need closer monitoring during dose titration. The Ozempic prescribing information advises monitoring those with a history of retinopathy. When discussing ozempic and eye problems with patients, emphasize routine optics checks, symptom tracking, and timely reporting of changes.
Monitoring Semaglutide and Vision: Practical Steps
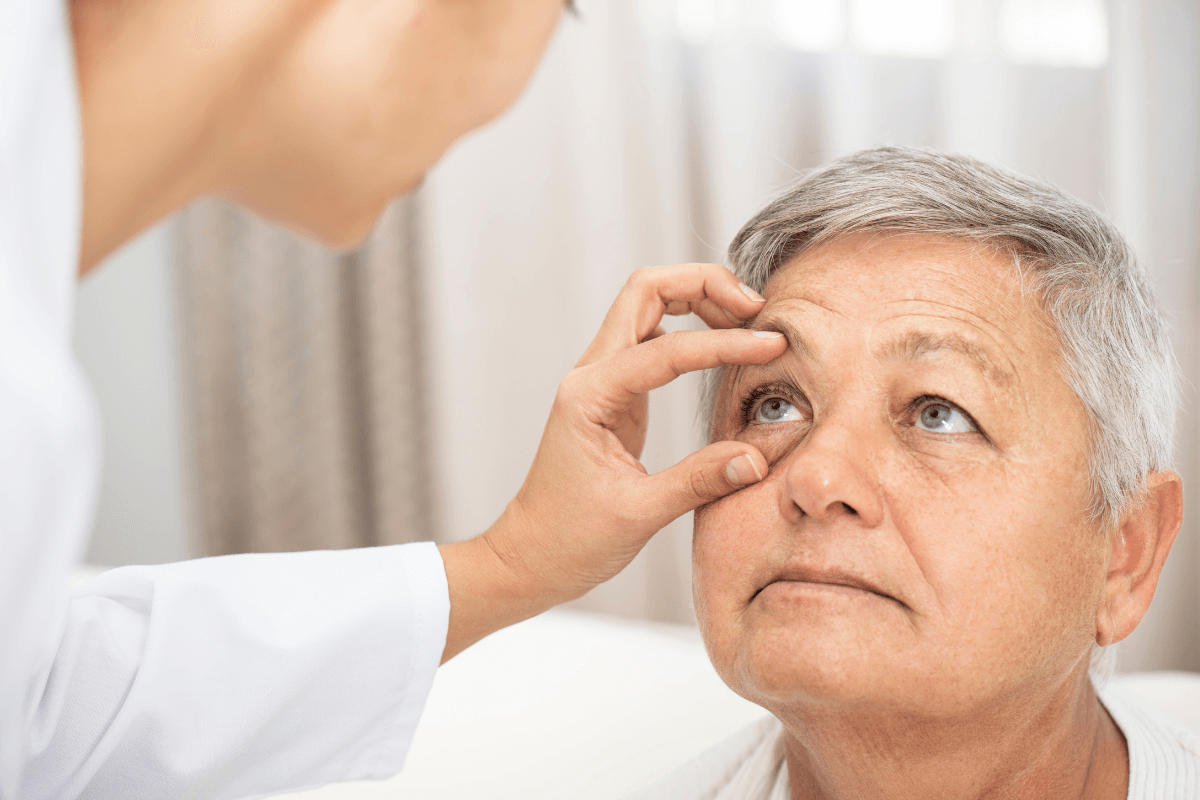
Set expectations early. Before or soon after starting treatment, arrange a dilated exam to document baseline findings. Share your medical history, including retinopathy, glaucoma, sleep apnea, migraines, and cardiovascular disease. Ask the eye team how often they recommend follow-up, and confirm who to call if symptoms change.
Keep a simple diary of any visual changes. Note date and time, dose changes, and coinciding factors such as illness, new medicines, dehydration, or heavy exertion. Bring this log to visits. If visual symptoms start suddenly, do not wait for a routine appointment—call for urgent assessment.
When to Call an Eye Specialist
Seek same-day evaluation for sudden vision loss, a curtain-like shadow, a burst of new floaters, eye pain with redness, or severe headache with visual symptoms. These signs can indicate retinal detachment, acute glaucoma, uveitis, or optic neuropathy, all of which warrant urgent care. Gradual blur can be monitored, but rapid change deserves faster attention. If you cannot reach your regular clinic, urgent care or emergency services can help triage eye emergencies.
People with diabetes should also confirm when their next dilated exam is due. If recent glucose changes were large, clinicians may schedule an earlier recheck. For prevention strategies tailored to diabetes eye health, see Diabetic Eye Disease Month for screening intervals and risk reduction tips, and review Managing Retinopathy In Diabetes for practical care steps.
Symptoms to Watch For and What They Might Mean
Several symptoms warrant attention during GLP-1 or GLP-1/GIP therapy. Some are benign and temporary, while others are true emergencies. Keep a written record and report all new or worsening changes promptly. Clear documentation helps clinicians judge whether symptoms relate to medications, fluctuating glucose, or something else.
- New floaters or flashes: Could signal posterior vitreous detachment or, rarely, a retinal tear.
- Central blur or distortion: Might reflect fluid shifts or macular disease; needs evaluation.
- Eye pain with redness: Consider acute glaucoma, uveitis, or corneal issues; urgent care needed.
- Sudden partial vision loss: Raises concern for retinal detachment or optic neuropathy.
- Gradual blur: Often accompanies changing A1C; still ask for timely review.
Patients often ask about ozempic eye side effects in general terms. Reassure them that most visual changes are mild and reversible, but do not downplay emergencies. For a refresher on how common medicines interact in diabetes care, see Common Diabetes Medications for mechanisms and class differences.
Who May Be at Higher Risk?
Risk is individual. Those with existing diabetic retinopathy, prior retinal procedures, severe hypertension, sleep apnea, glaucoma, high myopia, or vascular disease merit closer follow-up. Age, smoking history, and migraines may also factor into optic nerve vulnerability. Baseline exams help tailor timing and detect subtle changes early.
Although evidence remains limited, clinicians should keep rare optic neuropathies in mind, especially with sudden, painless vision loss. Use careful language when discussing semaglutide naion because causal links are not proven. Inform patients about warning signs and ensure they know how to access urgent care. For additional cardiometabolic context that may influence ocular risk, consider Mounjaro Heart Benefits for cardiovascular effects that intersect with eye perfusion.
How to Prepare for Eye Appointments and Document Changes
Preparation improves outcomes. Bring a current medication list, recent A1C, blood pressure readings, and your symptom diary. Note the timing of dosing, any titration steps, and other new prescriptions. Include over-the-counter products and supplements. Ask your clinician to summarize a plan for monitoring and who to contact for new symptoms.
Patients sometimes ask what are ozempic eyes when describing nonspecific blur or dryness. Encourage precise descriptions: onset, duration, one or both eyes, and triggers. Bring recent photos or screenshots if visual phenomena are easier to show than explain. For treatment timelines that may guide monitoring, see How Long Can You Take Ozempic for duration considerations that can shape follow-up spacing. Broader weight-management context is covered in GLP-1 Medications for balanced expectations during therapy.
Comparing GLP-1/GIP Agents on Ocular Signals
Evidence is still evolving across the class. Small differences in pharmacology, dose, and speed of glucose improvement may shape symptom patterns. Head-to-head ophthalmic safety data are sparse. For now, apply similar monitoring principles across GLP-1 and GLP-1/GIP agents, adjusting follow-up by individual risk and symptom severity.
Public conversation often groups these medicines together, yet the data are not identical. Reports of wegovy eye side effects remain limited, and stronger trials are needed. Product resources can support informed discussions; see Wegovy for drug background details, and Ozempic Semaglutide Pens for dosing forms and indications. For related cardiometabolic therapy context, explore Orforglipron vs Rybelsus to understand oral incretin options that may affect monitoring logistics.
Reporting Side Effects and Staying Safe
Online discussions, including threads about ozempic blurry vision reddit, are not a substitute for clinical assessment. If you suspect an adverse reaction, document details and contact your care team. You can also report events directly to regulators. This supports pharmacovigilance and helps researchers refine safety signals over time.
The U.S. Food and Drug Administration provides a simple reporting pathway. When symptoms are serious or unusual, file a report through FDA MedWatch with the timing, dose, and outcome. For additional side-effect education strategies, see Xultophy Side Effects to compare how clinicians frame monitoring for complex therapies. If you want broader topic updates, browse our Diabetes Articles category for ongoing coverage relevant to eye health.
Recap
Most GLP-1 users will not develop serious eye problems, but vigilance matters. Baseline and follow-up exams catch changes early, and clear action plans reduce risk. Keep symptom logs, ask targeted questions, and seek urgent care for red-flag signs. For regular updates across vision care, continue exploring our Ophthalmology resources for clinically focused guidance.
Note: If symptoms escalate suddenly, prioritize urgent evaluation rather than waiting for routine review.
This content is for informational purposes only and is not a substitute for professional medical advice.