Modern diabetes care depends on synthetic insulin. Today’s products mirror natural human insulin and are engineered for consistency, purity, and predictable action. Knowing what they are made of, how they are produced, and why methods evolved helps patients, caregivers, and students understand therapy choices and safety controls. We also connect the science with everyday use and practical storage and delivery considerations.
Key Takeaways
- Core material: Recombinant human protein, produced in microbes.
- Reliable process: DNA insertion, fermentation, and purification steps.
- Why it changed: Consistency and safety replaced animal sourcing.
- Design options: Analogs adjust onset, peak, and duration.
- Quality controls: Global standards help ensure product uniformity.
What Is Synthetic Insulin?
The term synthetic insulin refers to laboratory-produced insulin that matches, or purposefully modifies, the human hormone. Manufacturers program microbes to produce the insulin protein, then purify and formulate it for therapeutic use. These medicines include regular human insulin and insulin analogs designed for specific onset and duration needs. Both forms aim to support tight but safe glucose control.
Clinically, insulin is a peptide hormone that lowers blood glucose. It enables glucose uptake, inhibits liver glucose output, and coordinates fat and protein metabolism. In practical terms, that means fewer swings in blood sugar when dosed appropriately. Care teams often combine basal and mealtime doses to mimic the body’s normal patterns.
How Insulin Is Made: From DNA to Dose
At the core, manufacturers use recombinant DNA to program cells to make the insulin protein. To explain this process clearly, people often ask how is synthetic insulin made. First, scientists place the human insulin gene into a circular DNA vector. That vector goes into yeast or bacterial cells, which then express large amounts of insulin precursors during controlled fermentation.
Next, the insulin precursors are harvested and purified. Enzymatic and chemical steps help form the correct A and B chains and the necessary disulfide bonds. After polishing to remove impurities and endotoxin, the insulin is formulated with buffering agents, preservatives, and sometimes zinc or protamine. Final steps include sterile filling, labeling, and extensive lot testing before release.
Microbial Hosts and Purification Steps
Two host systems dominate: Escherichia coli and Saccharomyces cerevisiae. E. coli often produces insulin as inclusion bodies that require solubilization and refolding. Yeast tends to secrete the protein into the medium, simplifying some steps. Either way, manufacturers must achieve highly specific folding and bonding to reach native bioactivity. Chromatography, filtration, and refolding conditions are carefully tuned to preserve potency.
After purification, formulators blend stabilizers, adjust pH, and set ionic conditions to maintain consistency during storage. Pharmacopoeial tests confirm identity, purity, sterility, and absence of contaminants. These controls help ensure that each vial or pen behaves predictably, dose after dose. For a broader historical context on formulation shifts, see Evolution of Insulin Therapy for background on changes in action profiles.
Production Methods Then and Now
Before the 1980s, insulin primarily came from animal pancreases. Factory processes extracted, purified, and crystallized the hormone at scale. With the advent of recombinant DNA, how is insulin produced artificially shifted from slaughterhouse byproducts to precision bioprocessing. This transition improved lot-to-lot consistency and reduced immunogenic impurities, which matters for daily dosing reliability.
Today’s manufacturers operate bioreactors with tight control over temperature, nutrients, and oxygenation. Modern analytics monitor expression, folding, and aggregate formation in near real time. Once batches pass release criteria, cold-chain distribution maintains potency until use. For a deeper look at action duration in practice, the article Insulin Analogs explains how structural tweaks alter pharmacokinetics.
Historical Milestones and People
In the early 1920s, therapeutic insulin changed diabetes from a fatal condition to a treatable one. The contribution of frederick banting, alongside Charles Best, J.J.R. Macleod, and James Collip, marked a breakthrough that saved countless lives. The first human treatment occurred in 1922, and methods rapidly scaled afterward. Later, scientists used genetic engineering to produce human-sequence insulin without animal extraction.
For a concise overview of the discovery period, see The Discovery of Insulin for key dates and laboratory steps. To understand how delivery has changed from early glass syringes to pens and pumps, the guide Ways of Administering Insulin offers practical insights into modern options and technique.
Molecular Structure and Bioactivity
The structure of insulin consists of two peptide chains (A and B) linked by disulfide bonds. This arrangement is essential for receptor binding and signal transduction. In solution, insulin may form dimers or hexamers around zinc, which influences absorption after injection. Manufacturers exploit these properties to tune onset and duration through formulation changes.
Analogs alter select amino acids to affect self-association and tissue uptake. Rapid-acting analogs delay hexamer formation, speeding absorption. Long-acting analogs shift isoelectric points or form microprecipitates, extending release. For mechanistic examples, compare structural tweaks in Insulin Cartridges to understand packaging decisions that support stability.
What Insulin Does in the Body
The function of insulin is to facilitate glucose uptake into muscle and fat while suppressing hepatic glucose production. It also influences lipid storage, protein synthesis, and potassium balance. In everyday management, these actions help reduce hyperglycemia and limit metabolic complications. Dosing strategies aim to mirror physiologic patterns without causing hypoglycemia.
Different insulin types vary in onset and duration, which shapes mealtime and basal coverage. For comparative pharmacology on meal dosing, see Humulin vs Novolog for differences between human regular and rapid-acting analogs. For similar rapid-acting options, Novolog vs Humalog discusses how two analogs compare in timing and use scenarios.
From Animals to Recombinant: Why the Shift
Historically, much insulin was extracted from porcine or bovine pancreases. Over time, production moved to recombinant sources for purity, scalability, and ethical supply reasons. A key question often arises: why is pork insulin no longer used. The short answer is that recombinant products reduced variability and immunogenicity, and modern facilities can meet demand without relying on slaughterhouse waste streams.
Animal-sourced insulin remains relevant in veterinary practice. For example, protamine zinc formulations are used for cats and dogs. If you are exploring veterinary options, ProZinc Vial provides an overview of insulin specifically designed for pets, offered here to illustrate formulation differences across species.
Quality, Regulation, and Manufacturing Today
Across regions, regulators set standards for identity, purity, potency, and sterility. These expectations influence batch release, stability studies, and pharmacovigilance. To frame current practice, how is insulin made today involves validated bioprocesses, current Good Manufacturing Practices, and ongoing monitoring of lot consistency. Manufacturers test critical quality attributes to ensure predictable clinical performance.
For regulatory context, the U.S. agency outlines expectations for insulin products and their quality frameworks. For an introduction to oversight, the FDA provides insulin product information summarizing manufacturing and safety considerations. For patient-friendly explanations of action categories, the NIDDK offers types of insulin that relate formulation to timing and use.
Storage, Delivery, and Practical Use
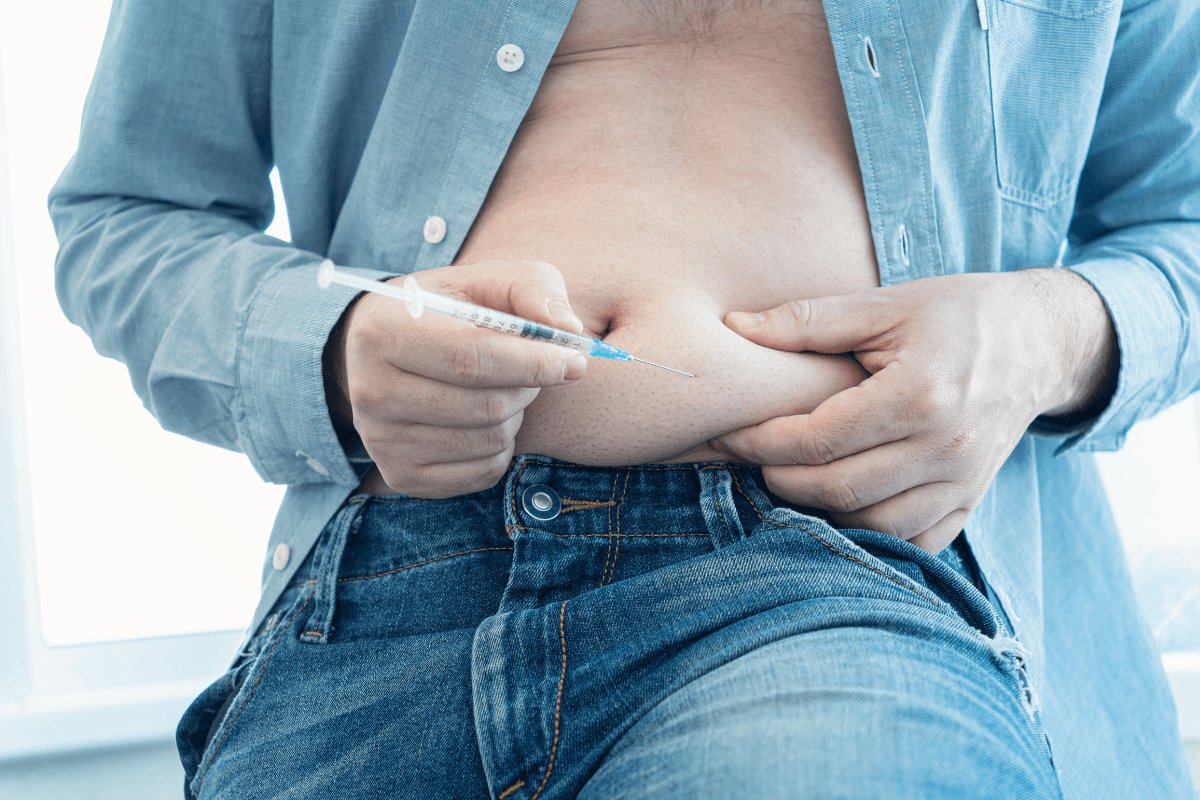
Insulin is stored naturally in pancreatic beta-cell granules, then secreted with rising glucose. Therapy aims to replace that dynamic pattern with scheduled dosing. Safe handling matters because exposure to heat, light, or freezing can impair potency. Knowing how devices work helps patients dose accurately and handle interruptions.
To compare administration routes and technique, see Ways of Administering Insulin for context on pens, syringes, and pumps. For device packaging and stability features, Insulin Cartridges explains materials and benefits in common systems. For a long-acting case study, Lantus Insulin Cartridge shows how steady-release formulations support basal coverage. Needle choice also affects comfort and technique; see BD Needles for gauge and length selection considerations.
Recap
Synthetic insulin is a recombinant human protein produced in controlled microbial systems, then purified and formulated for reliable clinical use. The shift from animal extraction to genetic engineering improved consistency, reduced impurities, and expanded capacity. Understanding DNA insertion, fermentation, and purification steps clarifies why modern products behave predictably across lots. Molecular design also matters: small sequence or formulation changes can change onset, peak, and duration to match real-life dosing needs.
Connecting history, manufacturing, and practical use helps patients and learners make sense of therapy options. If you want a broader overview of related topics, browse Diabetes Articles for technique, comparisons, and product guidance. Device-focused readers can also review Diabetes Products to understand delivery systems and components. Continue exploring linked guides to see how engineering choices translate into safe, predictable care.
This content is for informational purposes only and is not a substitute for professional medical advice.