Tresiba is an ultra–long-acting basal insulin (long-acting insulin) used to help control blood glucose. This overview focuses on tresiba uses, core dosing principles, pen technique, and safety considerations. It also outlines when alternatives or add-on therapies may be appropriate. Use this as a practical reference and discuss personal decisions with your healthcare professional.
Note: Do not change your insulin plan without medical guidance. Label recommendations and local standards may differ.
Key Takeaways
- Ultra–long action: once-daily basal with flexible timing.
- Dose carefully: titrate gradually and track glucose data.
- Safety first: prevent hypoglycemia and rotate injection sites.
- Device know-how: prime, verify dose, and use a fresh needle.
- Alternatives exist: consider other basal insulins or combinations.
Understanding tresiba uses and indications
Tresiba (insulin degludec) is indicated for improving glycemic control in people with diabetes. Clinically, it serves as basal insulin to cover background needs day and night. It may be used in type 1 diabetes alongside rapid-acting mealtime insulin. It may also be used alone or with other agents in type 2 diabetes. Age eligibility and specific indications follow the product label in your region.
The medication’s prolonged, steady profile helps reduce gaps between doses. That profile may support consistent fasting and overnight control. Always confirm local labeling for pediatric use, timing flexibility, and combination rules. For a quick brand overview of degludec products, see Insulin Degludec Brand Names, which summarizes naming conventions and presentations across markets.
Refer to the U.S. prescribing information for detailed indications and administration principles, as labeling clarifies age ranges and combination use U.S. prescribing information.
How Tresiba Works and Delivery Options
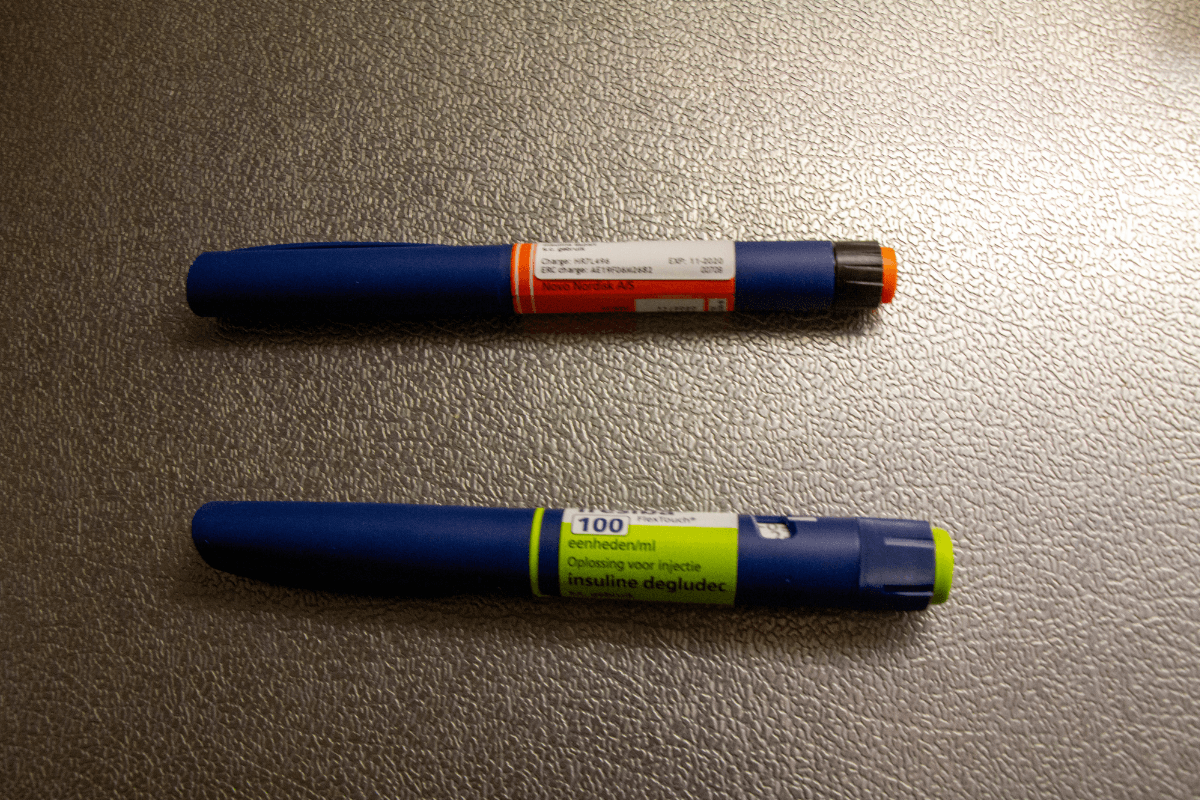
Tresiba forms a depot after subcutaneous injection, releasing insulin gradually (pharmacokinetics: how the body handles a drug). Its long duration provides a relatively flat basal effect in many users. The agent is available in prefilled pens and vials in some settings. Many adults prefer the pen format for simplicity and dose accuracy.
The common device is the tresiba flextouch pen, which clicks by units to help set doses precisely. Priming ensures insulin flow before each injection, and a fresh needle supports sterility and correct delivery. For a detailed feature overview, see Tresiba Flextouch Pen Usage, which covers design, priming, and dose windows. If you need device availability details, see Tresiba Flextouch Pens, which summarizes packaged strengths and formats.
Duration and flexibility are described in the official label, including practical instructions about missed doses and spacing between injections U.S. prescribing information.
Starting Dose and Titration Basics
Dosing should individualize based on glucose targets, hypoglycemia risk, and concurrent therapies. Clinicians often start basal insulin conservatively, adjusting every few days using fasting glucose trends. Many programs use small, stepwise increments to reduce hypoglycemia risk. Algorithms also consider lifestyle changes, steroid use, illness, and kidney function.
When discussing tresiba dosage, your care team may consider existing basal use, mealtime insulin needs, and overnight patterns. Flexible daily timing can help with adherence, but maintain adequate spacing, per label. Structured logs or glucose downloads guide dose adjustments and confirm stability. For dosing tables and label language, see Tresiba Uses, Dosage, Side Effects, which organizes typical titration steps and precautions.
Standards documents describe how to titrate basal insulin carefully, balancing fasting targets and hypoglycemia prevention ADA Standards of Care.
Safety Profile and Side Effects
Most people tolerate basal insulin well. The most common concern is hypoglycemia (low blood sugar), which can present with shakiness, sweating, confusion, or palpitations. Mild episodes may respond to fast carbohydrates; severe episodes may require emergency care. Injection site reactions, lipodystrophy (fat tissue changes), and weight gain can also occur.
Discuss new or worsening vision symptoms, edema, or redness at injection sites promptly. Some medicines, including GLP-1 receptor agonists or thiazolidinediones, may influence insulin needs or fluid status. If you experience tresiba side effects that disrupt daily life, contact your care team. For symptom patterns and mitigation tips, see Tresiba Side Effects Guide, which details monitoring strategies and when to escalate care.
Guidance documents cover hypoglycemia risk factors and general management steps; you can review current recommendations here ADA Standards of Care.
Comparing Basal Insulins
Several long-acting options exist, and choices depend on duration needs, variability, and personal preference. Topics like onset, peak profile, and device style matter. Differences in concentration or pen increments may influence ease of use. Switching between agents should follow label instructions and clinician guidance to reduce risk.
People often ask about tresiba vs lantus when optimizing a basal plan. Conversion can be near 1:1 in many scenarios, but medical oversight is essential, especially with timing changes or concurrent bolus insulin. For a point-by-point comparison, see Tresiba vs Lantus Guide, which outlines pharmacology, dosing, and device differences. For a broader context with another analog, see Tresiba vs Levemir, which contrasts duration and titration approaches. If you are evaluating alternatives, Lantus Solostar Pens provides a reference point for pen format and strength.
Practical Dosing Scenarios
Real life is messy. Travel, shift work, or illness can strain routines. When a dose is missed, the product label explains spacing rules and what to do next. Many users can dose when remembered and then resume the usual schedule, but spacing matters. Monitoring glucose more closely after any deviation is wise. Discuss a contingency plan with your clinician.
Patients sometimes ask about the maximum dose of tresiba. Some require higher units because of insulin resistance, steroids, or acute illness. Pens have maximum per-injection limits, and high daily totals may benefit from split strategies or adjunct therapies. If you accidentally take more than intended, increase monitoring and seek medical advice. Label instructions describe missed-dose handling and spacing requirements U.S. prescribing information.
Alternatives and Add-On Therapies
Basal insulin is one piece of comprehensive diabetes management. If fasting control remains unstable or doses escalate, your clinician may consider complementary agents. GLP-1 receptor agonists, SGLT2 inhibitors, or mealtime insulin can address postprandial spikes and reduce overall insulin need. Device selection, including pen style and increments, also shapes adherence and outcomes.
When weighing tresiba alternatives, discuss goals, hypoglycemia risk, cost, and supply. For those needing a combination approach with GLP-1 support, see Xultophy Prefilled Pen, which outlines the degludec–liraglutide pairing. If comparing against biosimilar glargine, Tresiba vs Basaglar explains practical differences during transitions. Broader class context is summarized in Insulin Analogs, which reviews mechanism and duration.
Using the Pen Correctly
Correct pen technique improves safety and consistency. Always prime before the dose to confirm insulin flow. Verify the dialed dose and hold the needle in place for several seconds after injection. Rotate injection sites across the abdomen, thighs, or upper arms to reduce tissue changes. Replace needles after each use to prevent blunting and contamination.
Questions about tresiba flextouch how to use are common among new users. The core steps include checking the label strength, priming, dialing the prescribed dose, and injecting into clean skin at a proper angle. Pen-specific instructions describe maximum per-injection volume and reading the dose counter. For a broader refresher on insulin types and delivery, see Different Types of Insulin, which compares basal and bolus roles.
Tip: Store unopened pens as directed. In-use pens typically stay at room temperature for a limited time; verify exact timeframes on the label.
Recap
Tresiba provides a stable basal option with flexible timing and pen convenience. Its long profile may help smooth fasting control when paired with personalized titration. Safety hinges on hypoglycemia prevention, careful adjustment, and solid technique. Alternatives or add-ons can be considered when goals are not met.
Use this overview to frame discussions with your clinician. Bring glucose logs, device questions, and treatment goals to each visit. That preparation helps tailor a plan that fits your routine and reduces risk over time.
This content is for informational purposes only and is not a substitute for professional medical advice.