Please note: a valid prescription is required for all prescription medication.
Tresiba FlexTouch Pens Uses, Dosage Basics, and Safety
Start 2026 with savings: Use code SAVE10 for 10% OFF all RX meds. Jan–1 Mar. Ozempic from Canada and Mounjaro Vial not included. Offer valid until March 1st. Coupon code cannot be combined with other offers. For products with “Bulk Savings”, the discount will be applied to the regular price for 1 unit. Maximum allowable quantity equal to a 90 day supply per single order.
Price range: $163.99 through $183.99
You save


Tresiba is a long-acting insulin (insulin degludec) supplied in prefilled pen devices. It is used as basal insulin to help control blood glucose in diabetes. This page summarizes dosing basics, safety, storage, and practical handling.
Some patients explore Ships from Canada to US when comparing refill options, depending on eligibility and jurisdiction. The goal is to support informed discussions with a clinician and safe day-to-day use alongside regular glucose monitoring.
What Tresiba FlexTouch Pens Is and How It Works
Tresiba FlexTouch Pens contain insulin degludec, a basal (background) insulin designed to provide steady glucose-lowering coverage over a full day and beyond. After injection under the skin, insulin degludec forms multi-hexamers (a slow-release depot), which helps extend its action and smooth out peaks compared with shorter-acting insulins. Basal insulin is typically used to cover the glucose your liver releases between meals and overnight, and it is often paired with mealtime insulin or non-insulin medicines when needed.
CanadianInsulin generally facilitates prescription referral and may confirm prescription details with the prescriber when required. Understanding how basal insulin works can also help you compare options within browseable hubs such as Long Acting Insulin and condition collections like Diabetes. For broader context on therapy classes, the guide Common Diabetes Medications summarizes how insulin and non-insulin treatments fit together.
Why it matters: Basal insulin helps manage glucose when you are not eating.
Who It’s For
This medicine is indicated to improve glycemic control in adults and pediatric patients with diabetes mellitus, and it may be part of care for both Type 1 Diabetes and Type 2 Diabetes. In type 1 diabetes, basal insulin is used alongside rapid-acting mealtime insulin. In type 2 diabetes, it may be used alone or combined with other glucose-lowering therapies depending on a clinician’s plan, A1C goals, and hypoglycemia risk.
It is not used to treat diabetic ketoacidosis (DKA), which requires urgent medical management and different insulin strategies. Tresiba is not for intravenous use and is not intended for insulin pump therapy. A key contraindication is a known serious hypersensitivity to insulin degludec or any component of the formulation. People with repeated severe low blood sugar episodes, significant visual impairment, or limited ability to recognize symptoms of hypoglycemia may need additional safety planning with their care team.
Dosage and Usage
Follow the prescribing clinician’s instructions and the product label for dose, timing, and titration. In general, insulin degludec is administered once daily by subcutaneous injection, and some patients may be instructed to take it at the same time each day to support routine. If a dose is missed, labeling for many patients includes taking the missed dose when remembered and then returning to the usual schedule, while ensuring adequate time between doses; individual instructions can differ based on the overall regimen and glucose patterns.
Before injecting, check the pen label and inspect the solution (it should be clear and colorless). Rotate injection sites within the same region to reduce lipodystrophy (fatty tissue changes) and skin thickening, which can affect absorption. Do not share pens, even if the needle is changed, because blood-borne infection risk remains. If you want a broader view of insulin choices that may be listed alongside other diabetes therapies, the navigation hub Insulin Medications can be a helpful starting point for comparing categories and forms.
Quick tip: Keep a simple log of injection time and site region.
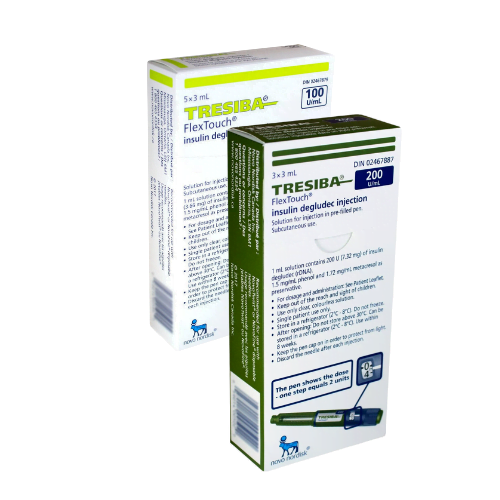
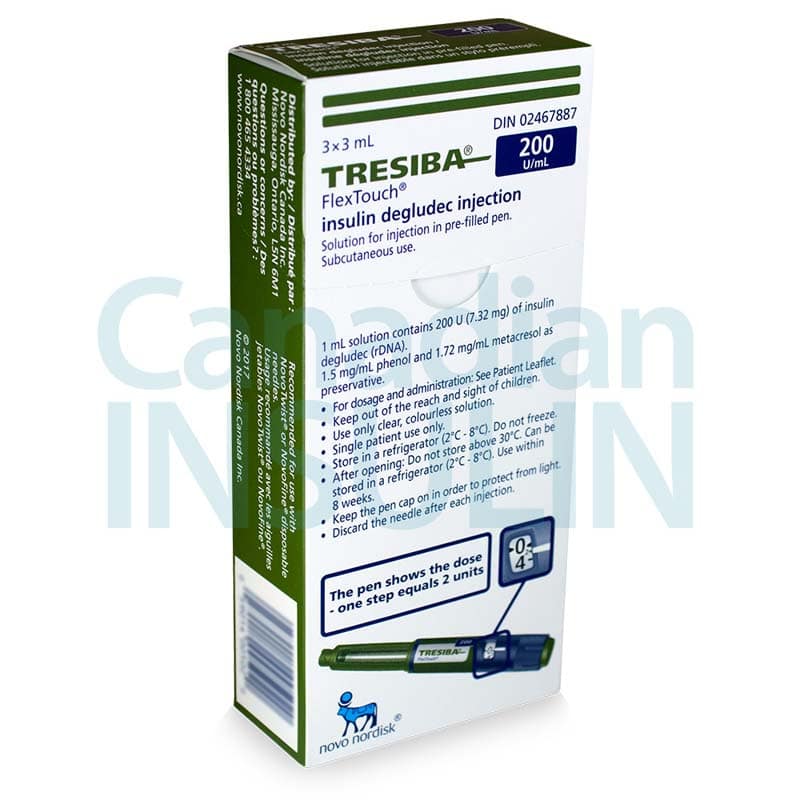
Strengths and Forms
Tresiba FlexTouch Pens are prefilled injection pens that typically contain 3 mL of insulin solution. They are available in different concentrations, and the concentration affects how many insulin units are delivered per mL. Because the device may look similar across strengths, it is important to confirm both the concentration and the dose window before first use, and to avoid switching strengths unless the prescriber specifically directs it.
Availability can vary by jurisdiction and pharmacy partner. Common presentations include U-100 (100 units/mL) and U-200 (200 units/mL), which are both insulin degludec but are not interchangeable unit-for-unit without guidance on device selection and patient technique. The table below summarizes typical forms:
| Form | Concentration | Device |
|---|---|---|
| U-100 pen | 100 units/mL | Prefilled pen, 3 mL |
| U-200 pen | 200 units/mL | Prefilled pen, 3 mL |
For an overview of diabetes treatment formats (pens, vials, tablets, and injectables), the reference list Diabetes Medications List provides a high-level map of common options.
Storage and Travel Basics
Store unopened pens as directed on the label, commonly under refrigeration, and do not freeze. If a pen has been frozen, it should not be used. Protect insulin from excessive heat and direct light, including in cars, near windows, or next to heating vents. For day-to-day handling, keep the pen cap on when not in use, and avoid storing the pen with a needle attached because this can allow air to enter and insulin to leak.
After first use, many patients keep the in-use pen at room temperature within the labeled limits, and discard it after the manufacturer’s in-use time window, even if insulin remains. When traveling across time zones, insulin timing can become confusing; it is reasonable to plan ahead with a clinician or diabetes educator on how to maintain basal coverage safely. For additional practical reading and topic browsing, Diabetes Articles and Type 1 Diabetes Articles can provide background education that complements the official label.
Side Effects and Safety
The most important safety risk with any insulin is hypoglycemia (low blood sugar). Symptoms may include sweating, shakiness, fast heartbeat, hunger, confusion, headache, or irritability, and severe episodes can cause seizures or loss of consciousness. Risk can increase with missed meals, unexpected physical activity, alcohol intake, vomiting or diarrhea, dosing errors, or changes in kidney or liver function. Because basal insulin continues to act between meals, it is especially important to recognize patterns of overnight or fasting lows and discuss them with a clinician rather than making self-directed dose changes.
Other potential effects include injection-site reactions (redness, pain, itching), rash, or swelling. Weight gain can occur with insulin therapy in some people, often related to improved glucose utilization and reduced glycosuria. Rare but serious allergic reactions can occur; seek urgent care for signs such as generalized hives, difficulty breathing, or swelling of the face or throat. Insulin can also lower potassium (hypokalemia), which may be clinically relevant in people taking certain diuretics or with other risk factors. Ongoing monitoring typically includes home glucose checks and periodic lab follow-up (such as A1C), tailored to the overall treatment plan.
Drug Interactions and Cautions
Many medicines can change insulin needs by affecting glucose production, insulin sensitivity, appetite, or how quickly glucose enters the bloodstream. Examples that may raise glucose include systemic corticosteroids, some antipsychotics, and certain hormonal therapies. Medicines that may increase hypoglycemia risk include other glucose-lowering agents; alcohol can also contribute to unpredictable lows, especially if meals are delayed. Beta-blockers may mask some warning signs of low blood sugar (such as tremor and palpitations), which can delay recognition.
Thiazolidinediones (TZDs) used with insulin can increase the risk of fluid retention and heart failure in susceptible patients, so clinicians often monitor for swelling, shortness of breath, and rapid weight gain. Illness, stress, and changes in diet or exercise can also alter glucose patterns; in these situations, the safest step is usually to follow a clinician’s sick-day plan and monitor more closely. For browsing related condition and therapy hubs, the category pages Diabetes Products and Diabetes Medications can help you see how different medication types are organized.
Compare With Alternatives
Basal insulin options differ by active ingredient, duration, dose flexibility, device, and how they fit into a complete regimen. Alternatives that clinicians commonly consider include insulin glargine (available in multiple branded and biosimilar forms), insulin detemir in some regions, and NPH insulin, which generally has a shorter duration and more pronounced peak than newer long-acting analogs. The “best” choice is individualized based on glucose targets, hypoglycemia history, renal function, dosing convenience, and insurance coverage rules.
For type 2 diabetes, clinicians may also add or prioritize non-insulin therapies that address weight and post-meal glucose, such as GLP-1 receptor agonists, depending on patient-specific goals and contraindications. Examples on the site include Ozempic Semaglutide Pens and Rybelsus Semaglutide Pills, which are not basal insulins but may be discussed as part of combination care in appropriate patients. If injection technique is a concern across different injectables, the practical guide Mounjaro Injection Sites offers general, safety-focused pointers that may complement clinician instruction.
Pricing and Access
Coverage and out-of-pocket expense for insulin can vary widely by plan design, formulary placement, and whether a prior authorization is required. Some people consider Tresiba FlexTouch Pens as a cash-pay option when coverage is limited; others rely on private or public insurance rules. Documentation requirements can also vary, especially when a prescription needs clarification on concentration (U-100 vs U-200), quantity, or directions.
CanadianInsulin operates as a prescription referral service, and dispensing is handled by licensed third-party pharmacies where permitted by law. Depending on jurisdiction and eligibility, cross-border fulfillment may be considered as part of the process. For general, non-time-limited information that may apply to certain medications, see Promotions Page. If you are comparing options without insurance, it can help to ask a clinic staff member to confirm the exact product, concentration, and pen count written on the prescription so the correct item is reviewed.
When coordinating temperature-sensitive medicines, pharmacies may use prompt, express, cold-chain shipping as clinically appropriate.
Authoritative Sources
For the most accurate and current prescribing details, use the official prescribing information and reputable medical references.
- DailyMed listing for Tresiba labeling
- MedlinePlus overview for insulin degludec
- American Diabetes Association resources and standards
This content is for informational purposes only and is not a substitute for professional medical advice.
Express Shipping - from $25.00
Shipping with this method takes 3-5 days
Prices:
- Dry-Packed Products $25.00
- Cold-Packed Products $35.00
Standard Shipping - $15.00
Shipping with this method takes 5-10 days
Prices:
- Dry-Packed Products $15.00
- Not available for Cold-Packed products
What is Tresiba used for in diabetes care?
Tresiba (insulin degludec) is a long-acting, once-daily basal insulin used to improve blood glucose control in people with diabetes mellitus. “Basal” means it helps cover the body’s background insulin needs between meals and overnight. In type 1 diabetes, it is typically used with rapid-acting insulin taken at meals. In type 2 diabetes, it may be used alone or combined with other diabetes medicines, depending on a clinician’s plan and monitoring results. It is not used to treat diabetic ketoacidosis.
How is Tresiba different from mealtime insulin?
Mealtime (rapid-acting) insulin is designed to work quickly to cover the rise in glucose after eating. Basal insulin like insulin degludec is designed to work slowly and steadily to manage glucose release from the liver when you are not eating. Because the roles are different, the two types are often used together in type 1 diabetes and sometimes in type 2 diabetes. Mixing up basal and mealtime insulin can lead to significant hypoglycemia or hyperglycemia, so label and device checks are important.
Can I switch between U-100 and U-200 pens?
U-100 and U-200 are different concentrations (100 units/mL vs 200 units/mL). The pen device is designed to deliver insulin units, but switching strengths still requires clinician direction to avoid dosing errors and to ensure the correct pen is dispensed and taught. Confusion can happen because pens may look similar. If a prescriber changes the concentration, ask for clear written instructions on the exact product name, concentration, and dose in units, and confirm what to do with any remaining supply.
What are common side effects and serious safety concerns?
The most common and clinically important risk with insulin is hypoglycemia (low blood sugar). Mild symptoms may include sweating, shakiness, hunger, headache, or confusion. Severe hypoglycemia can cause seizures or loss of consciousness and needs urgent help. Other possible effects include injection-site reactions, skin thickening or dents from repeated injections in the same area, and weight gain in some people. Rarely, serious allergic reactions can occur. Ongoing glucose monitoring and reviewing patterns with a clinician support safer use.
What should I do if I miss a dose of basal insulin?
Missed-dose instructions can vary by product labeling and by a person’s overall regimen (for example, whether they also use mealtime insulin). Many patients are advised to take a missed basal dose when remembered, then return to the usual schedule while keeping adequate time between doses, but this is not universal. Because missed doses can lead to high glucose and “catch-up” dosing can increase hypoglycemia risk, it is safest to follow the prescriber’s written plan and contact the clinic if you are unsure.
How should an in-use insulin pen be stored?
Storage directions depend on the specific pen and the manufacturer’s labeling. In general, unopened pens are stored refrigerated and must not be frozen. After first use, many insulin pens can be kept at room temperature within labeled limits and should be discarded after a specified number of days or weeks, even if insulin remains. Keep the cap on to protect from light, and avoid storing the pen with a needle attached to reduce leakage and contamination risk. Always confirm the current instructions on the package insert.
What should I ask my clinician before starting or refilling insulin degludec?
Useful questions include: which concentration (U-100 or U-200) is intended; what dose in units and what time of day to take it; how to handle missed doses; what glucose targets and monitoring schedule to use; and how to recognize and treat hypoglycemia. Also ask about changes that can alter insulin needs, such as kidney disease, liver disease, steroid treatment, changes in diet or activity, or alcohol use. If you use other diabetes medicines, confirm how they fit with basal insulin and what side effects to watch for.
Rewards Program
Earn points on birthdays, product orders, reviews, friend referrals, and more! Enjoy your medication at unparalleled discounts while reaping rewards for every step you take with us.
You can read more about rewards here.
POINT VALUE
How to earn points
- 1Create an account and start earning.
- 2Earn points every time you shop or perform certain actions.
- 3Redeem points for exclusive discounts.
You Might Also Like
Related Articles
SGLT2 Inhibitors Explained: Uses, Risks, and Examples
Key Takeaways These medicines lower blood sugar by acting in the kidneys. Some are also labeled for heart failure or chronic kidney disease. Drug names include dapagliflozin, empagliflozin, and canagliflozin.…
Out Of Pocket Cost For GLP-1 Medications: Planning Tips
Key Takeaways Costs vary by drug, indication, and dose form Cash-pay totals include more than the pen Programs exist, but eligibility is limited Be cautious with compounded versions and unverifiable…
Rural Health Disparities Statistics To Compare Care Gaps
Key Takeaways Define “rural” before comparing outcomes across places. Use age-adjusted rates and stable time windows. Pair health metrics with access and capacity markers. Check small-number limits and data suppression…
DPP-4 Inhibitors Brand Names: Generics, Combos, Tips
Overview If you are sorting medications for type 2 diabetes, names get confusing fast. Lists often mix generics, trademarks, and short-hand. This guide breaks down dpp-4 inhibitors brand names and…