Choosing a basal insulin can feel technical. Levemir vs Lantus comparisons help clarify day-to-day differences, switching considerations, and safety points. This overview uses clinical terms and plain language so you can discuss options with your care team. We highlight dosing patterns, duration, and practical monitoring without giving medical advice.
Key Takeaways
- Two long-acting options: both detemir and glargine provide basal coverage.
- Different durations: glargine often lasts longer and more evenly.
- Switching requires caution: monitor closely after any basal change.
- Side effects overlap: hypoglycemia and weight changes can occur.
Levemir vs Lantus: Clinical Similarities and Differences
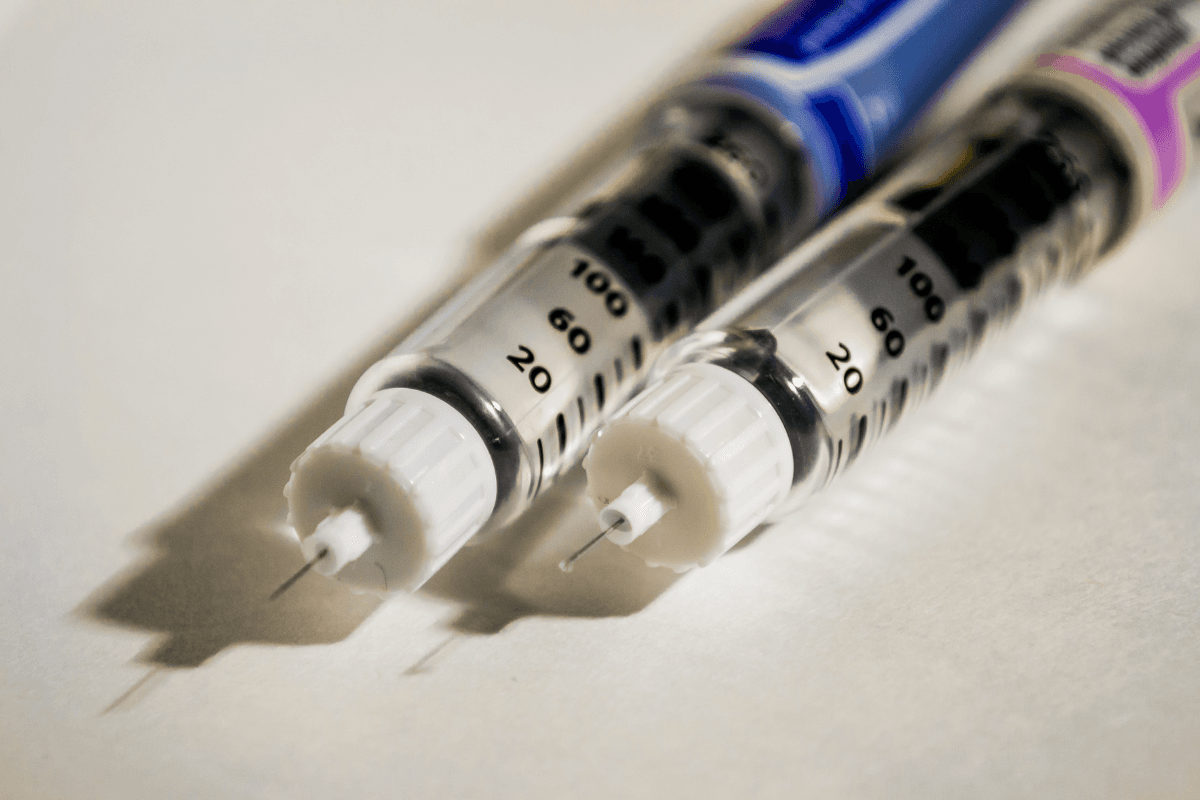
Both medicines are long-acting basal insulins designed to keep glucose steady between meals and overnight. Levemir (insulin detemir) often needs once- or twice-daily dosing. Lantus (insulin glargine) generally uses once-daily dosing in many adults. Pharmacology differs, but each aims for a consistent background effect.
Neither product replaces mealtime insulin when rapid control is needed. However, they may be combined with prandial insulin in basal–bolus regimens for Type 1 or Type 2 diabetes. For a broader overview of basal strategies, see Basal Insulin Types for indications and titration concepts. For glargine’s mechanism and profile, see How Lantus Works for absorption and activity details.
Pharmacokinetics and Dosing Patterns
In clinical practice, levemir vs lantus duration of action differs by patient, dose, and injection site. Glargine commonly provides near 24-hour coverage with a relatively peakless profile. Detemir’s effect may shorten at lower doses, leading some patients to use split dosing for full coverage. Individual variability matters, so expect adjustments based on fasting patterns and nocturnal readings.
Product labeling outlines kinetics and safety. For detemir’s prescribing information, see this insulin detemir label with onset and duration details. For glargine’s prescribing information, review the insulin glargine label for pharmacokinetics and safety sections. For detemir timing specifics, see Insulin Detemir Duration to compare onset, peak, and duration.
Switching Between Basal Insulins
Changing basal insulin should be individualized and monitored. Some clinicians may consider a cautious levemir to lantus conversion 1:1 in selected stable adults, then adjust using fasting glucose trends. Even with similar total units, day-to-day glucose variability can change after the switch. Expect to reassess fasting patterns, nocturnal lows, and morning highs within days of any adjustment.
Guideline statements emphasize safety and close follow-up. For evidence-based context, see the ADA Standards of Care on pharmacologic approaches. For background on basal titration frameworks, see Basal Insulin Types for starting points and safety checks. If switching from or to other long-acting options, you may also compare profiles using Tresiba vs Lantus for duration and dose-timing considerations.
Safety Profile and Side Effects
Across trials and clinical experience, lantus vs levemir side effects are broadly similar. Hypoglycemia remains the main risk, particularly with missed meals, increased activity, or renal changes. Injection-site reactions and mild edema can occur. Rarely, insulin antibodies may influence dose requirements and variability.
Weight change varies by patient and co-therapies. Lifestyle, concurrent medications, and hypoglycemia prevention strategies influence trends. For a focused overview, see Levemir Side Effects for adverse event patterns and monitoring tips. For detemir-specific onset and reactions, see Insulin Detemir Duration for expected timing and precautions.
Special Situations: Pregnancy and Weight Considerations
Evidence for levemir vs lantus in pregnancy continues to evolve. Detemir has supportive clinical data in pregnant patients with diabetes, while glargine data are more limited but growing. Both require careful monitoring and obstetric coordination. Dose needs may increase during pregnancy and fall after delivery, so plans should anticipate dynamic insulin sensitivity.
Weight considerations matter with any insulin therapy. Small weight increases can occur from reduced glycosuria and hypoglycemia avoidance snacks. Discuss goals, nutrition, and activity with your care team. For pregnancy management frameworks and medication selection, see the relevant sections of the ADA Standards of Care for risk–benefit context and monitoring guidance.
Interchangeability, Biosimilars, and Alternatives
In practice, formulary coverage and clinical fit both drive choices. Comparisons like levemir vs lantus vs basaglar help clarify whether a biosimilar glargine suits your plan. Basaglar is a follow-on glargine product with comparable clinical use. For formulation details, see Basaglar Cartridge for device specifics and handling notes.
Some people move to ultralong options with flatter profiles. When reviewing alternatives, look at duration needs, nocturnal patterns, and dose timing tolerances. For broader comparisons with degludec, see Tresiba vs Lantus to understand profile differences and clinical trade-offs. Discuss whether a switch would simplify your schedule or complicate other parts of your regimen.
Practical Tools, Calculators, and Monitoring
Some clinicians reference an insulin conversion calculator when planning cautious basal changes. These tools can summarize common switch scenarios, yet they do not replace individualized clinical judgment. If you explore calculators for converting Levemir to Lantus, confirm assumptions like target fasting ranges and monitoring windows.
Other tools may outline NPH-to-glargine or degludec-to-glargine conversions. Use them as starting points, then individualize based on readings and hypoglycemia risk. For detemir-specific dosing context, see Levemir Insulin Dosage Guide for titration basics. For storage guidance after dispensing, see Levemir FlexPen Storage for room-temperature limits and reminders.
Cost and Access Considerations
Insurance coverage and local formularies often shape choices. Discussions about lantus vs levemir cost should consider total monthly units, device format, and any biosimilar options. Device convenience and availability also matter. Prefilled pens may reduce user error, while vials can suit people using syringes or pumps.
When budgets are tight, explore support programs and covered biosimilars. A less expensive alternative to detemir may be a glargine follow-on, if clinically appropriate. If needles or sites are a concern, review technique and rotation. For placement advice and comfort strategies, see Levemir Injection Sites for rotation patterns and site selection tips.
Practical Use: Technique, Timing, and Follow-Up
Stable technique helps reduce variability. Inject at consistent times, rotate sites, and review fasting glucose patterns weekly. Record shifts in appetite, exercise, and sleep that could change insulin needs. After any change, prioritize conservative adjustments and increased monitoring over several days.
Tip: Keep a simple log during transitions. Note dose time, site, units, and any overnight lows. Share these details at follow-up. For background on how glargine behaves in the body, see How Lantus Works for absorption concepts. For broad reading across topics, browse Diabetes Articles for technique, safety, and device guides.
Recap
Both detemir and glargine provide basal coverage, yet profiles differ. Duration, dosing frequency, and device format can guide your choice. Switching requires cautious plans and close monitoring. Use tools to structure the conversation, then tailor decisions to your readings and goals.
Note: If you are comparing delivery devices or cartridges, review handling instructions on the product page or device leaflet before use.
This content is for informational purposes only and is not a substitute for professional medical advice.