Most people first hear about insulinoma during an evaluation for unexplained low blood sugar. This rare pancreatic tumor drives excess insulin release, causing recurrent hypoglycemia that can be confusing and dangerous. Understanding the biology, tests, and therapies helps you plan safer daily routines and informed discussions with your care team.
Key Takeaways
- Rare beta-cell tumor that causes recurrent hypoglycemia.
- Diagnosis rests on supervised fasting tests and biochemical markers.
- Surgery often offers definitive control when feasible.
- Medical therapy manages symptoms when surgery is not possible.
- Ongoing monitoring reduces relapse risk and emergency events.
What Is Insulinoma?
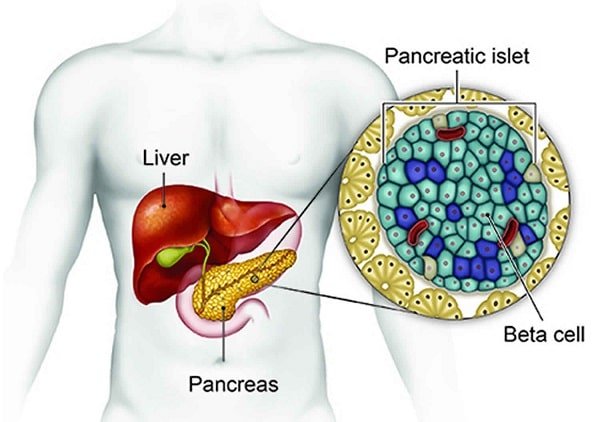
This pancreatic neuroendocrine tumor arises from beta cells, which normally regulate insulin. Excess hormone release lowers blood glucose, producing neuroglycopenic (brain-related) and adrenergic (stress-response) symptoms. Most tumors are small and solitary. Many are benign, but a minority behave aggressively and spread to lymph nodes or the liver.
Clinicians often refer to Whipple’s triad: symptoms of hypoglycemia, a low measured plasma glucose, and relief after glucose is given. This framework helps distinguish true hypoglycemia from look‑alike conditions. For a concise public summary of pathophysiology and care, see the NIDDK overview (NIDDK overview), which aligns with contemporary guidance.
Root Causes and Risk Factors
Most cases occur sporadically without a clear trigger. However, inherited syndromes, particularly multiple endocrine neoplasia type 1 (MEN1), raise the lifetime risk. In these families, tumors can be multiple and appear earlier. Age typically ranges from mid‑adulthood onward, though younger adults are occasionally affected.
Proposed mechanisms include dysregulated beta‑cell signaling and growth pathways that favor autonomous insulin secretion. Environmental causes are not well defined. When discussing insulinoma causes, clinicians balance genetics, tumor biology, and individual metabolic context. People with MEN1 often receive periodic screening because early detection can simplify management and lower complications.
Clinical Signs and Early Clues
Neuroglycopenic symptoms—confusion, blurred vision, speech difficulty, or behavior changes—often dominate. Adrenergic signs, such as tremor, palpitations, anxiety, and sweating, may precede or accompany cognitive changes. Episodes commonly occur in the early morning, after exercise, after fasting, or after alcohol intake.
Some individuals experience morning headaches, frequent naps, and increased appetite. Recurrent snacking to relieve lows can lead to gradual weight gain. Typical symptoms of insulinoma vary by glucose nadirs and episode frequency. Family or coworkers may notice personality shifts or brief periods of unresponsiveness during severe episodes.
How Doctors Confirm the Diagnosis
Evaluation begins with a careful history of timing, triggers, and relief patterns. Laboratory assessment during spontaneous symptoms is ideal. When spontaneous sampling is not possible, clinicians may perform a supervised fasting protocol. This controlled setting allows safe monitoring while confirming biochemical criteria and excluding alternative causes.
Imaging focuses on locating very small pancreatic lesions. High‑resolution CT, MRI, and endoscopic ultrasound each contribute different advantages. For background on fasting patterns and differential causes, see our practical explainer Fasting Hypoglycemia, which outlines when prolonged testing is considered and how results are interpreted.
C‑Peptide and Related Markers
When glucose is low, paired measurements of insulin, C‑peptide, and proinsulin clarify endogenous secretion. Elevated values in this state support excessive beta‑cell activity. Clinicians may also review beta‑hydroxybutyrate suppression and response to glucagon. These biochemical fingerprints strengthen the case before any procedure.
Documentation of insulinoma diagnosis c-peptide improves confidence that insulin is coming from the pancreas rather than outside sources. For a clinician‑focused summary of diagnostic criteria and differential diagnosis, the StatPearls review (peer‑reviewed overview) provides detailed algorithms and caveats.
Medical Therapy and Tumor Control
When surgery is delayed or not possible, clinicians aim to reduce hypoglycemia burden and protect daily function. Dietary strategies prioritize frequent, balanced meals with complex carbohydrates, protein, and fiber. Carefully timed snacks before activity or sleep may help reduce overnight lows.
Pharmacologic insulinoma treatment may include diazoxide to limit insulin release and somatostatin analogs when appropriate. In select advanced cases, targeted therapies can suppress hormone output and slow growth. For broader hormone‑excess context, our Hyperinsulinemia Guide explains why symptom patterns fluctuate across days and situations.
Preparedness matters during a severe low. For immediate reversal plans, discuss keeping a Glucagon Injection Kit near areas where episodes tend to occur. Some patients prefer needle‑free administration; for that scenario, learn about Baqsimi Nasal Powder and how caregivers can administer it quickly.
Definitive Surgical Management
When feasible, insulinoma surgery offers the best chance of durable control. Many solitary tumors are removed by enucleation, sparing most pancreatic tissue. Deeper or strategically located tumors may require distal pancreatectomy or, rarely, more extensive resections. Minimally invasive approaches are common in experienced centers.
Preoperative localization blends cross‑sectional imaging with endoscopic ultrasound, which detects small lesions. Intraoperative ultrasound further guides precise resection. After surgery, teams watch for transient hyperglycemia or pancreatic leak. For broader endocrine oncology context, browse our Endocrine & Thyroid collection, which explains how endocrine tumors can present and be managed across systems.
Prognosis, Follow‑Up, and Outcomes
Outcomes vary with tumor size, number, and pathology. After complete resection of localized disease, many patients enjoy long symptom‑free periods. Regular follow‑up assesses glucose stability and screens for recurrence with labs and targeted imaging when indicated.
When disease is metastatic or unresectable, goals shift to symptom control and quality of life. Reported insulinoma survival rate figures vary across studies and case mix, reflecting the rarity of this condition. A multidisciplinary plan helps coordinate nutrition, medications, and monitoring to reduce emergency visits and maintain independence.
Dogs: Presentation, Care, and Quality of Life
Veterinary presentations share many parallels with people, including episodic weakness, disorientation, collapse, and seizure-like activity. Care teams use fasting tests, imaging, and response to therapy to confirm the diagnosis. Early recognition and consistent routines help reduce dangerous dips and improve daily comfort for pets.
Owners often ask about insulinoma in dogs life expectancy. Longevity depends on tumor stage, surgical success, and response to medical therapy. Advanced cases may experience progressive neurological signs and reduced activity tolerance. For a comprehensive pet-focused discussion, see our companion guide Insulinoma in Dogs, which explains home monitoring, feeding strategies, and veterinary follow‑up.
Metabolic Effects on the Liver
Chronic hyperinsulinemia can suppress hepatic glucose production, particularly during fasting. The liver normally releases stored glycogen and generates new glucose to keep levels steady. When insulin remains inappropriately high, this counterregulatory support diminishes, and lows become more frequent or more severe.
In parallel, ketone production falls, limiting an alternative brain fuel source during hypoglycemia. This helps explain why some episodes feel abrupt and intense. For an overview contrasting causes of low glucose in different conditions, our side‑by‑side explainer Hypoglycemia vs. Diabetes outlines how management strategies adapt across settings.
Daily Safety, Nutrition, and Monitoring
Structured routines reduce risk. Many teams recommend a balanced breakfast within an hour of waking, followed by planned snacks ahead of long meetings, driving, or workouts. Alcohol increases hypoglycemia risk; pair drinks with food and monitor closely.
Continuous glucose monitoring can help some patients recognize patterns and respond earlier. Keep a written action plan that lists symptoms to watch for, steps to take, and when to seek help. For related metabolic context, see Diagnosing Insulin Resistance to understand how insulin dynamics shape your responses across the day.
Caregiver Coordination and Emergency Planning
Brief training for family, friends, or coworkers can prevent injuries during severe hypoglycemia. Teach how to check responsiveness, place the person on their side if needed, avoid forced oral intake when not fully alert, and administer rescue glucagon if prescribed. Label storage locations clearly and review expiration dates. After recovery, eating a complex carbohydrate plus protein helps stabilize levels. For lifestyle adjustments that complement medical care, our article Living With Diabetes shares practical routines and mindset tips that can improve day‑to‑day stability.
Recap
This tumor’s hallmark is recurrent hypoglycemia driven by endogenous insulin. Confirmation relies on paired biochemistry and careful localization. Surgery can be curative when feasible; medical measures help when it is not. Plan nutrition, monitoring, and emergency preparedness to lower risk, and maintain regular follow‑up with your care team.
Note: For general cancer‑focused reading, our curated Cancer Articles provide broader context on tumor behavior, terminology, and care pathways, which may help during multidisciplinary consultations.
This content is for informational purposes only and is not a substitute for professional medical advice.