Understanding Calcium and Diabetes helps you connect basic mineral biology with everyday glucose management. This guide explains mechanisms, clinical signs of imbalance, diet vs supplements, and practical monitoring steps.
Key Takeaways
- Core mechanism: calcium drives insulin release and muscle uptake.
- Dyscalcemia may worsen glycemia or mimic diabetic complications.
- Prioritize food sources; supplement only when indicated.
- Check labs and medications that shift calcium balance.
Calcium and Diabetes: Core Mechanisms and Clinical Context
Calcium ions trigger insulin secretion in pancreatic beta cells and support insulin-sensitive glucose uptake in muscle. Disturbances in calcium handling may therefore influence fasting glucose, post‑meal spikes, and overall variability. The effect is modest, but it can matter when combined with diet, activity, and medications.
Glucose outcomes depend on multiple intertwined factors, including kidney function, vitamin D status, and hormone signals like parathyroid hormone. In clinical settings, small calcium shifts often accompany acute illness, diuretic use, or dehydration. These shifts may complicate interpretation of fingerstick or CGM readings, especially during intercurrent illness.
Calcium Signaling, Insulin Secretion, and Sensitivity
Insulin release depends on calcium influx into beta cells, and muscle glucose uptake requires normal ion gradients. This physiological link explains the relationship between calcium and glucose across fasting and postprandial states. It does not mean more calcium always improves glycemia; balance and context drive outcomes.
Several diabetes medications alter appetite, gastric emptying, or renal handling and may indirectly influence mineral balance. For a concise overview of pharmacologic actions that shape glycemia, see Common Diabetes Medications And How They Work for mechanism summaries that help frame monitoring decisions. Coordinating diet, medications, and labs reduces confounding when glucose patterns change unexpectedly.
Practical Implications for Daily Management
Day to day, aim for consistent calcium intake and adequate hydration. Combine resistance exercise with balanced meals to support insulin sensitivity and muscle calcium handling. Track glucose after major dietary changes, new supplements, or medication adjustments. If readings drift, check for missed doses, intercurrent illness, or diuretics that increase urinary calcium.
When patterns persist, discuss basic labs (serum calcium, albumin, magnesium, and renal panel) with a clinician. Reviewing medication lists is equally important. Thiazide diuretics can raise calcium, while loop diuretics can lower it. Document symptoms, timing, and glucose data to guide targeted evaluation rather than broad trial‑and‑error changes.
Dyscalcemia in Diabetes: Signs, Labs, and Differential
Low calcium can cause muscle cramps, tingling, and facial twitching. These low calcium symptoms may overlap with neuropathy complaints, so a brief lab check can prevent misattribution. Always interpret total calcium alongside albumin or use ionized calcium when available.
Chronic kidney disease, common in diabetes, disrupts calcium‑phosphate‑vitamin D balance and raises fracture risk. For context on renal complications that intersect with mineral metabolism, see Diabetes And Kidney Damage for mechanisms and monitoring priorities. If bone pain, recurrent fractures, or unexplained fatigue occur, broaden testing to vitamin D, PTH, and phosphate as clinically indicated.
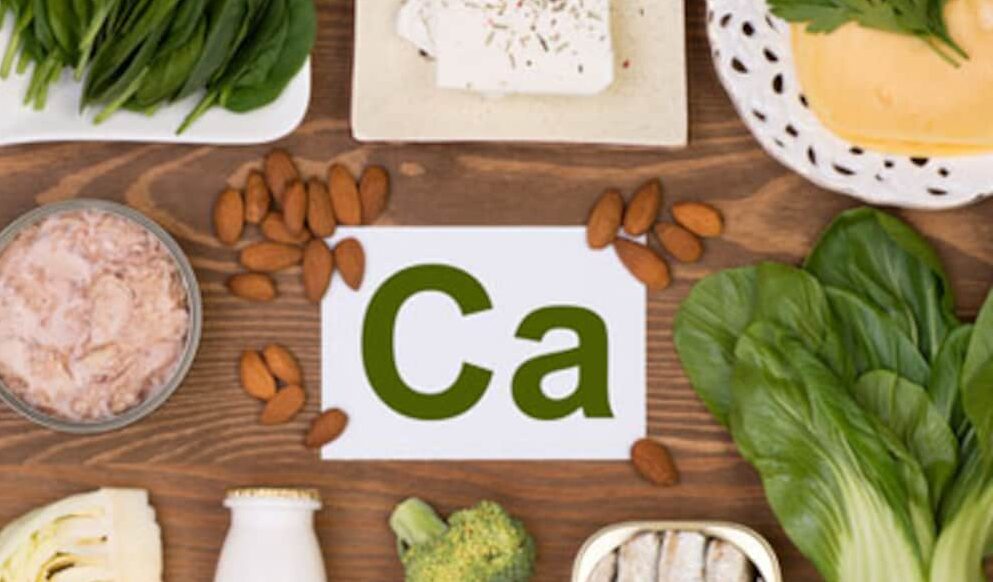
When nutrition is limited, consider calcium‑rich foods before supplements. Dairy, fortified plant milks, tofu, and leafy greens provide absorbable calcium with additional nutrients. For food planning ideas that fit glucose goals, see Diabetes Friendly Dairy for protein and calcium options, and Tofu For Diabetics Nutrition And Benefits for fortified choices suitable for lactose intolerance.
Hypercalcemia, Cancer Clues, and Parathyroid Disease
Sustained high calcium can reflect dehydration, excess intake, medication effects, hyperparathyroidism, or malignancy. People often ask whether is high calcium a sign of cancer. Cancer is one possible cause, but most cases stem from primary hyperparathyroidism or medications; clinicians look at trends, PTH, and imaging to refine the cause.
If labs suggest parathyroid overactivity, further evaluation clarifies severity and treatment options. For a concise clinical primer, the hyperparathyroidism overview provides etiology and diagnostic pathways. Key hypercalcemia symptoms and red flags are outlined in this hypercalcemia guidance, which also notes when urgent evaluation is warranted.
Type‑Specific Considerations and Comorbidities
The physiology of calcium intersects with both autoimmune and insulin‑resistant states. In discussions of calcium and diabetes type 2, consider how insulin resistance, obesity, and fatty liver alter hormonal signaling. Sleep apnea, chronic kidney disease, and hypertension may add layers that complicate calcium balance and glucose control.
People with type 1 diabetes also face bone health concerns driven by autoimmune disease duration and glycemic variability. For broader bone risk context in diabetes, see The Fragile Connection Between Diabetes And Bone Fractures for fracture patterns, and Bone Problems Associated With Diabetes for skeletal complications. Managing blood pressure also matters; for related cardiovascular considerations, see Low Blood Pressure Hypertension And Diabetes to understand overlapping risks and treatments.
Diet, Supplements, and Safe Use
Food first remains the safest strategy. Dairy, sardines with bones, fortified soy or almond milk, tofu set with calcium, and leafy greens distribute intake across the day. People often ask how much calcium should a diabetic take. Needs usually mirror general recommendations and depend on age, sex, kidney function, and dietary pattern; discuss personal targets with a clinician.
Excess supplemental calcium may raise kidney stone risk, cause constipation, or interfere with iron and thyroid medication absorption. For evidence‑based intake ranges and upper limits, see the NIH calcium fact sheet for age‑specific guidance used in clinical practice. If you do use a supplement, divide doses to improve absorption and reduce gastrointestinal side effects.
Choosing a Supplement Wisely
Calcium carbonate is cost‑effective and best absorbed with meals, while calcium citrate is better when stomach acid is low or when taking acid‑suppressing therapy. Check labels for elemental calcium per tablet and avoid exceeding the tolerable upper intake without supervision. Separate calcium from iron or levothyroxine by several hours to minimize interactions. For a broader view of supportive products and nutrients, see Vitamins & Supplements for formulations and combinations that align with dietary gaps.
Diet planning benefits from dairy and fortified options if tolerated. For practical grocery choices that fit glycemic goals, visit Diabetes Friendly Dairy for protein‑rich foods that supply calcium naturally. Plant‑forward eaters can review Almond Milk And Diabetes to compare fortified beverages used in meal plans.
Vitamin D, Magnesium, and Bone Health
Vitamin D supports intestinal calcium absorption and bone turnover, while magnesium stabilizes ATP‑dependent enzymes and parathyroid hormone dynamics. In practice, clinicians sometimes evaluate calcium and vitamin d for diabetes when bone density is low or dietary intake is inconsistent. Correcting deficiencies may improve musculoskeletal outcomes even if glycemic effects are small.
When considering supplements, align choices with bone density findings, fracture history, and kidney function. For vitamin D’s metabolic context, see Vitamin D And Diabetes for links to insulin sensitivity and immune signaling. For injury prevention habits that protect bone, review Bone And Joint Health Awareness for posture, strength, and fall‑prevention tips.
Practical Monitoring and When to Seek Care
New symptoms, medication changes, dehydration, or acute illness can shift calcium levels. Patients sometimes ask, does insulin decrease calcium levels, but standard doses usually do not drive clinically meaningful calcium changes. Instead, look for diuretics, vitamin D dosing, immobilization, or kidney function changes when calcium results are abnormal.
If gastrointestinal slowing or appetite changes alter nutrient intake, review glucose goals and labs with your clinician. For background on GLP‑1 therapies that may influence appetite or gastric emptying, see Rybelsus Semaglutide Pills to understand their role in diabetes care. To keep learning across topics, browse Vitamins Supplements and Diabetes for related educational articles assembled by theme.
Recap
Calcium influences insulin secretion, muscle uptake, and bone health, while diabetes and its treatments can shift mineral balance. Most people meet needs through food; supplements fill gaps when labs or diet indicate a shortfall. Consistent intake, adequate vitamin D, and attention to medications support stability.
Use labs, symptoms, and medication reviews to target problems rather than guessing. When calcium is persistently high or low, evaluate with a clinician for reversible causes such as dehydration, diuretics, vitamin D dosing, hyperparathyroidism, or renal disease. A measured approach helps you manage glucose while protecting bones and kidneys.
Note: External references in this article are provided for general education and may not reflect personalized medical guidance.
This content is for informational purposes only and is not a substitute for professional medical advice.