Key Takeaways
- Rapid-acting option: Helps cover meals and correct high glucose.
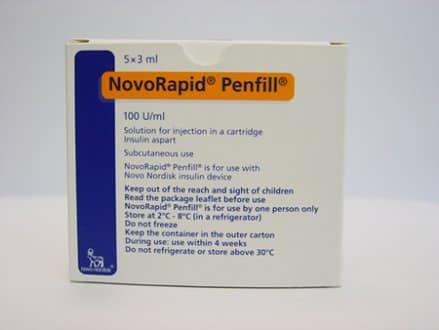
- Formats differ: PenFill fits reusable pens; FlexPen is disposable.
- Dosing is individualized: Use ratios, correction factors, and logs.
- Safety first: Watch for hypoglycemia, stacking, and site rotation.
- Storage matters: Respect temperature limits to maintain potency.
Managing mealtime insulin works best with clear, consistent steps. People using novorapid insulin aspart often need practical guidance on timing, dose frameworks, and monitoring. This guide outlines how the medication works, ways to use PenFill and FlexPen, and what to watch for with side effects.
Understanding Novorapid Insulin Aspart
Novorapid is a rapid-acting insulin analog used for mealtime coverage and corrections. It starts working quickly, helping glucose move from the bloodstream into cells. Clinicians often pair it with a long-acting insulin as part of basal-bolus therapy. This approach can improve flexibility around meals and activity.
Insulin aspart has a fast onset and a relatively short duration. Those kinetics support pre-meal dosing and targeted corrections. For more detail on onset and peak profiles, see Insulin Aspart Onset and Duration for timing ranges and monitoring notes. You can also review international product information; the European product overview summarizes pharmacology and safety in plain terms.
PenFill and FlexPen: Formats and Everyday Use
PenFill cartridges fit into compatible reusable devices and allow dose dialing and cartridge changes. FlexPen comes prefilled and disposable, which may simplify use for many people. Both formats require priming, consistent injection technique, and regular site rotation. Proper technique helps limit variability and discomfort.
In different markets, the insulin aspart brand name may vary, which can cause confusion when switching supplies. Check cartridge compatibility and pen needle length before starting a new box. For device background and cartridge mechanics, see our Insulin Cartridges Guide for insertion steps and troubleshooting pointers. If you use Novorapid cartridges, our Cartridge Use With Novorapid offers fit checks and practical tips. For storage specifics on prefilled pens, see FlexPen Storage Guidelines for temperature limits and in-use timelines.
Dosing Principles and Practical Charts
Dosing should be individualized by your healthcare professional. Most people use carbohydrate ratios to match mealtime intake and a correction factor to address high readings. Keep written logs of doses, meals, and activity. Those records help your clinician refine targets and reduce variability.
Some patients use an aspart insulin dosage chart to organize typical meal doses and correction steps. Charts should reflect your current insulin-to-carbohydrate ratio, correction factor, and target glucose. They also need routine updates when patterns change. For additional background on safe corrections and dose limits, our Dosage and Overdose Overview explains warning signs and when to seek care.
Sample Mealtime Framework
Start with your prescribed insulin-to-carbohydrate ratio, such as 1 unit per 10–15 grams of carbohydrate. Calculate mealtime insulin by dividing carbs by your ratio. If glucose is above your target, add a correction based on your sensitivity factor. Subtract insulin only if using active insulin on board is appropriate for your plan. Log each dose alongside carbohydrate counts and activity. Bring your records to follow-up visits so your clinician can adjust your regimen safely and precisely.
Timing With Meals
Timing affects control and safety. Many people inject shortly before eating to match rise in glucose after the first bites. Others may adjust timing if meals are unpredictable or delayed. Discuss timing changes with your healthcare team when patterns shift.
Guidance often addresses insulin aspart before or after meal decisions when pre-bolusing is difficult. A consistent routine helps reduce highs and lows. For nuance on rapid-acting options, compare profiles in Novorapid vs. Humalog to understand practical differences in onset and duration. You can also explore Vial Handling for Novorapid for additional preparation and dosing context.
Maximum Dose and Safety Limits
There is no single universal cap for rapid-acting insulin because requirements vary widely. Clinicians individualize totals using weight, insulin resistance, and glucose patterns. That said, higher mealtime doses may increase hypoglycemia risk if meals are missed or delayed. Consider split dosing for unusually large meals under professional guidance.
Plans sometimes reference an insulin aspart maximum daily dose to set a personalized upper boundary. That boundary helps prevent stacking and supports safer corrections on high-glucose days. The FDA drug overview for insulin aspart provides official labeling and safety information for prescribers and patients. Always confirm dose changes with your clinician before altering your regimen.
Side Effects and Monitoring
Common issues include hypoglycemia, injection-site reactions, lipodystrophy, and mild weight gain. Symptoms of low glucose include shakiness, sweating, headache, and confusion. Severe lows can cause seizures or loss of consciousness and require urgent treatment. Keep glucose tablets or another quick source of carbohydrate available.
Clinicians also review less common risks like hypokalemia and allergic reactions. Report rash, wheezing, swelling, or severe pain at the injection site. Understanding novorapid insulin side effects helps you recognize problems early and respond quickly. For a broader view across brands, see Novolog Side Effects for symptom patterns and escalation steps. MedlinePlus provides accessible summaries; see the insulin aspart overview for safety details and patient instructions.
Contraindications and Interactions
The most important insulin aspart contraindications include use during hypoglycemia and known hypersensitivity to insulin aspart or excipients. Caution is needed with conditions that change insulin needs, such as acute illness, renal impairment, or hepatic impairment. Dosing may need close supervision during these times to reduce risk of hypoglycemia.
Certain medications can mask or alter hypoglycemia symptoms. Beta-blockers may blunt warning signs such as tremor and tachycardia. Thiazolidinediones can increase fluid retention when combined with insulin. Review your medication list with your healthcare professional during each visit. Official sources like the European product overview summarize interaction cautions and special populations clearly.
Patient Teaching and Nursing Points
Education supports consistency and safety. Emphasize site rotation, needle changes, and priming before each injection. Review hypoglycemia recognition and treatment steps at every visit. Patients should know when to check ketones, especially during illness or persistent hyperglycemia.
Effective insulin aspart nursing considerations include reinforcing dose calculation steps and documenting active insulin on board. Encourage patients to carry identification and a source of fast-acting carbohydrate. For broader condition education, our Type 1 Diabetes and Type 2 Diabetes hubs collect treatment basics and monitoring guides. Tip: Keep a small written checklist for dose timing, site, and post-meal checks to reduce omissions.
Storage, Handling, and Travel
Store unopened pens and cartridges in the refrigerator within labeled temperature limits. Avoid freezing and protect from heat and direct light. Once in use, many pens can be kept at room temperature for a specified period. Always follow the format-specific in-use timelines on the label or patient leaflet.
When traveling, carry insulin in hand luggage with a cooling wallet if needed. Keep a backup pen, extra needles, and a copy of prescriptions. For cartridge-specific handling, review our Cartridge Use With Novorapid for storage thresholds and carry tips. Storage differences between vials, cartridges, and pens are outlined in Insulin Cartridges Guide to help prevent potency loss.
Rapid-Acting Alternatives and Comparisons
Several rapid-acting options exist with similar roles but different kinetics. Fiasp (faster aspart) may have a quicker onset for some patients. Humalog (insulin lispro) and Apidra (insulin glulisine) are other alternatives. Your clinician can help choose based on response, preferences, and insurance.
To understand brand similarities and differences, see Novorapid vs. Novolog for formulation and unit equivalence notes. For pen-device considerations, the SoloStar Pen Overview gives design context you can compare with FlexPen. Fiasp’s practical advantages during workouts are discussed in Faster Aspart Cartridges to support active schedules.
Recap
Novorapid supports flexible mealtime coverage when dosing and timing match your routine. Choose the right format, follow safe calculation steps, and monitor closely. Use logs, site rotation, and clear storage rules to keep therapy steady. Discuss any changes with your clinician before adjusting doses or schedules.
Note: Official labeling offers the most current safety details. Review the FDA drug overview and the European product overview when confirming timing, storage, and risk information.
This content is for informational purposes only and is not a substitute for professional medical advice.