Understanding rapid acting insulin helps you plan meals, activities, and glucose checks with fewer surprises. This guide reviews timing, peaks, and brand examples in clear, practical terms.
Key Takeaways
- Onset and peak matter most for meals and corrections.
- Analog options act faster than older regular formulations.
- Basal insulins aim for flat coverage with minimal peaks.
- Absorption varies by site, dose, and activity level.
- Always confirm label specifics for your exact product.
How Rapid Acting Insulin Works: Onset, Peak, Duration
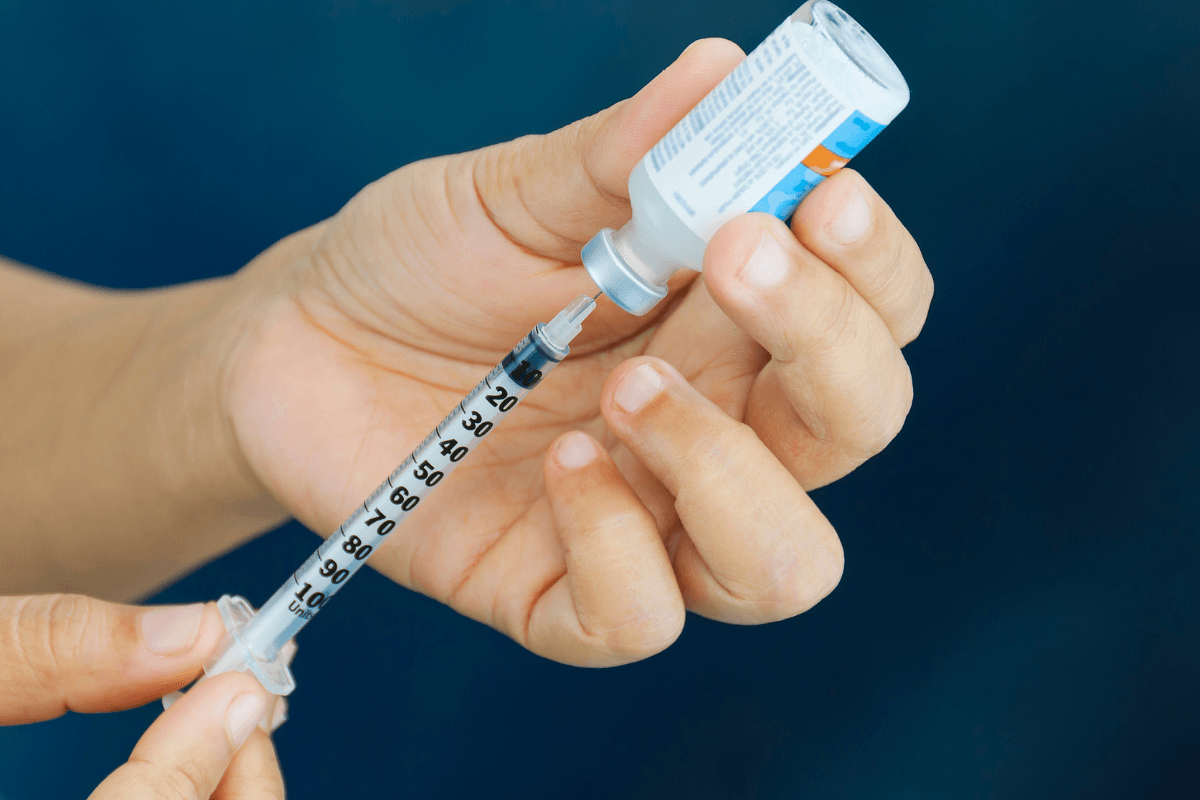
Rapid-acting analogs are designed for quick absorption and short action. They help manage post-meal glucose rises and correction doses. In clinical terms, this class provides prandial bolus insulin (mealtime coverage) with a relatively early peak effect. Common examples include insulin aspart, lispro, and glulisine.
Most products start lowering glucose within minutes, peak roughly one to three hours after injection, and wear off within several hours. Timing varies by formulation and individual factors. Faster aspart can begin working earlier than standard aspart, while lispro may resemble aspart timing in many users. To understand category roles further, see Basal vs Bolus Insulin for a concise comparison of background and mealtime coverage.
For authoritative timing ranges, the ADA Standards of Care summarize insulin categories and typical profiles across products (ADA Standards of Care).
Basal vs Bolus Insulin offers a clear primer on how mealtime doses differ from background insulin coverage, which helps when planning schedules.
Insulin Timing at a Glance: Onset and Peaks
The insulin peak times chart below condenses typical onset, peak, and duration by class. Ranges reflect common label values and clinical guidance. Your response can differ, so use these as orientation, not absolute rules.
| Type | Onset | Peak | Duration | Examples |
|---|---|---|---|---|
| Rapid-acting analogs | 5–15 minutes | 1–3 hours | 3–5 hours | Aspart (Fiasp/NovoRapid), Lispro (Humalog), Glulisine (Apidra) |
| Regular (short-acting) | 30–60 minutes | 2–4 hours | 5–8 hours | Humulin R, Novolin Toronto |
| Intermediate (NPH) | 1–3 hours | 4–12 hours | 12–18 hours | Humulin N/NPH, Novolin N |
| Long-acting basals | 1–2 hours | Minimal/flat | Up to ~24 hours | Glargine (Lantus), Detemir (Levemir) |
| Ultra-long basals | 1–2 hours | Minimal/flat | ~42 hours or longer | Degludec (Tresiba) |
Reference profiles vary between manufacturers and regulators. For product-specific onset and peak, consult the official label. As one example, faster aspart’s timing differences are described in the manufacturer’s prescribing information (Novo Nordisk labeling). Broader product differences are also summarized in our internal overview, which compares categories and formulations in plain language.
For context across brands and categories, the Insulin Products Guide highlights how formulation changes alter absorption and effect.
Short and Intermediate Insulins: Practical Differences
Older regular formulations have slower onset and later peaks than newer analogs. This timing means you may need a longer interval between injection and eating. Regular products can still be useful where cost, availability, or specific clinical needs guide therapy. However, they often require more planning around mealtimes.
Intermediate-acting insulin sits between short and basal options. It tends to have a noticeable peak and a longer tail. Because of that peak, some patients time meals or snacks to match the rising effect. Dose splitting and schedule consistency can help minimize variability.
For a brand comparison within rapid-acting choices, see Apidra vs Humalog for practical contrasts in usage and flexibility.
Tip: Regular insulin peak is later than rapid analogs, so plan pre-meal timing accordingly when switching.
NPH Details and Timing Nuances
Neutral protamine Hagedorn (NPH) uses protamine to delay absorption. That delay creates a clear peak, which can increase variability and the risk of nocturnal hypoglycemia (low blood sugar). Many people still use NPH due to familiarity or coverage needs, but careful timing and consistent carbohydrate intake can help reduce swings.
In some plans, NPH is paired with mealtime analogs or used in premixed products. If you use mixes, understand each component’s timing and the proportions. For a concise overview of how fixed-ratio mixes behave during the day, see Premixed Insulin for key scheduling points and practical caveats.
Note: Always verify label specifics and discuss changes with a clinician. Official product information provides the definitive timing and safety details (FDA drug database).
Basal Options: Long and Ultra-Long
Basal insulins aim to provide steady background coverage with minimal peaks. Modern analog basals typically have smoother curves than NPH. They help cover fasting needs and between-meal glucose output. Because they are less peaky, they can reduce nocturnal hypoglycemia compared with older intermediate options, while still requiring careful monitoring.
Ultra-long formulations extend coverage even further, which may support flexible dosing windows and fewer missed-dose gaps. They can be helpful when daily schedules vary or when a very flat profile is needed. For a broader context on medicines used with basal therapy, see Common Diabetes Medications for how non-insulin agents complement background insulin effects.
Authoritative guidance on class timing and safety appears in professional resources; for example, the ADA provides regularly updated practice recommendations (ADA Standards of Care).
Brands and Devices: What You’ll See
Rapid-acting analog brands include aspart (NovoRapid and faster aspart/Fiasp), lispro (Humalog), and glulisine (Apidra). These are available as vials, cartridges for reusable pens, and disposable pens. Device choice affects convenience and dosing granularity but does not fundamentally change pharmacology. Many users prefer pens for portability and smaller dosing steps.
Basal analog brands include glargine, detemir, and degludec. Pens and cartridges improve ease of use, and some lines offer junior or half-unit options. If you are comparing delivery formats, the article on Insulin Cartridges explains how cartridges fit reusable pens, while Humalog Insulin Pen reviews a common pen platform and its dose increments.
For specific devices within the aspart family, see Novorapid Cartridge when considering cartridge-based setups and Humalog KwikPen when evaluating disposable pen options—both linked here to illustrate device variety.
Dosing and Timing: Safety First
Consistency helps make absorption more predictable. Rotating injection sites within a region, matching dose timing to meals, and accounting for recent activity can all affect glucose outcomes. Larger doses may absorb more slowly, while lipodystrophy areas can cause erratic uptake. Tracking patterns over several days often reveals timing issues.
Basal and mealtime schedules differ in type 1 and type 2 diabetes. Background insulin addresses fasting needs, while prandial doses cover carbohydrate exposure and corrections. For broader context on routines and education topics, browse Type 1 Diabetes resources for common pattern-management themes relevant to daily care.
When adjusting routines, consider how meals, alcohol, and exercise interact with absorption. If you change devices or formulations, recheck timing assumptions. For general dose-planning frameworks, see the Insulin Dosage Chart for terminology and structure used in clinical discussions.
Real-World Examples and Meal Scenarios
Imagine an early lunch with moderate carbs. A modern analog dose given shortly before eating may blunt the glucose rise within the first few hours. Activity after the meal could accelerate absorption and increase the immediate effect, so extra monitoring is prudent during and after exercise.
Consider a late dinner with higher fat content. Absorption can feel different because fats slow gastric emptying, shifting the glucose curve later. In such cases, people sometimes notice that rapid acting insulin peak does not align with the delayed rise, requiring closer observation. Review recent logs before deciding how to stage doses around such meals.
Recap
Insulin timing is a blend of product design and real-life variables. Understanding onset, peak, and duration helps you match doses to meals and routines. Brands and devices add choice, while tables and labels anchor expectations. Use this knowledge to frame discussions with your care team and to interpret your daily readings.
This content is for informational purposes only and is not a substitute for professional medical advice.