Key Takeaways
- Most kidney cysts are simple and low risk.
- Complex features or rapid growth need specialist review.
- Blood sugar, blood pressure, and eGFR guide care.
- Genetic forms (HNF1B) can affect multiple organs.
Many people with kidney cysts also live with diabetes. Understanding how these conditions interact helps you plan monitoring, reduce complications, and time referrals. Clinicians sometimes call the combined pattern renal cysts and diabetes syndrome, often linked to HNF1B-related disease.
Understanding Renal Cysts and Diabetes Syndrome (RCAD)
RCAD describes a pattern of kidney changes with diabetes due to variants in the HNF1B gene. The condition may present with renal cysts, impaired insulin secretion, or both. Signs can vary widely, even within families. Some individuals develop mild kidney issues, while others progress to chronic kidney disease.
In clinical practice, RCAD is considered when cysts occur alongside early-onset diabetes, low magnesium, or structural urinary tract anomalies. A careful history, family context, and accessible genetic counseling can clarify whether HNF1B testing is reasonable. This discussion also frames expectations for surveillance of kidney function and metabolic health.
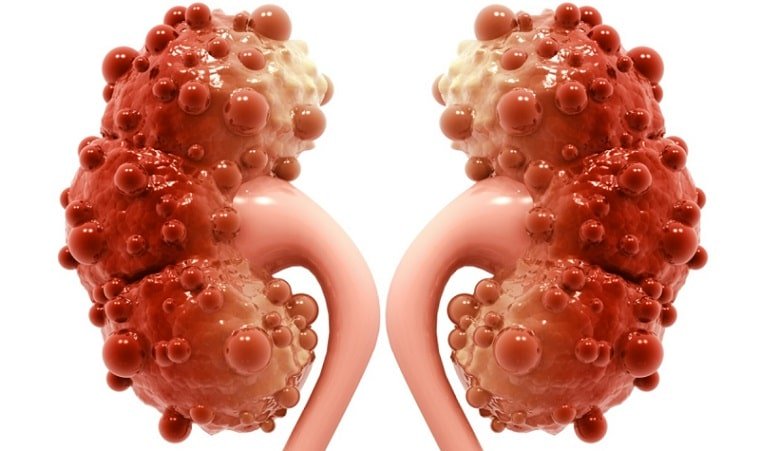
Causes and Types of Renal Cysts
Simple cysts usually arise with age from weakened tubule segments. They appear round, fluid-filled, and thin-walled on imaging. Complex cysts may have septations, calcifications, or enhancing solid areas. These features matter because they change follow-up intervals and the likelihood of intervention. When diabetes coexists, microvascular disease and hypertension can accelerate kidney stress, even if cysts remain incidental.
Inherited syndromes, prior infection, and obstructive uropathy can also contribute to cyst formation. Understanding kidney cyst causes helps tailor the workup and avoid unnecessary procedures. For an overview of simple versus complex cysts and expected imaging features, the National Institute of Diabetes and Digestive and Kidney Diseases provides clear guidance (NIDDK simple kidney cysts). For broader kidney-focused reading, see Nephrology for condition-specific articles, and Diabetes for metabolic care context.
When Size Becomes Risky: Imaging and Thresholds
Size matters most when paired with complexity and growth. A common clinical question is what size of kidney cyst is dangerous. There is no single cut-off, but radiologists apply structured criteria such as the Bosniak classification to categorize risk and set follow-up intervals. Complex features carry more weight than diameter alone, though very large cysts may cause pain or obstruction.
Imaging modality choice depends on context. Ultrasound is often first line; contrast-enhanced CT or MRI helps characterize borderline or complex lesions. To understand how radiologists grade cysts, see this patient-friendly overview of the Bosniak system from RadiologyInfo (Bosniak classification basics). When diabetes and kidney disease coexist, kidney-protective therapies may be relevant; for context on SGLT2 use in CKD, review Jardiance for Kidney Disease for potential renal support discussions.
Symptoms and Red Flags
Most simple cysts cause no symptoms. When present, renal cyst symptoms can include flank discomfort, a palpable mass, urinary changes, or fever if infected. Hematuria and uncontrolled pain warrant timely evaluation. Sudden, severe pain may reflect cyst rupture, hemorrhage, or obstruction and needs urgent assessment.
Systemic signs matter too. Rising blood pressure, declining eGFR, or recurrent urinary infections can signal complications. ACE inhibitors can support kidney protection in appropriate patients; for related background, see Benazepril Uses for kidney and blood pressure considerations. Always align medication choices with comorbidities and current lab trends.
Sex-Specific Considerations
Symptom patterns can differ by sex and life stage. For example, kidney cyst symptoms in females may be noticed during pregnancy workups or pelvic imaging. Pregnancy introduces hemodynamic and hormonal changes that can unmask urinary tract issues. Shared care between obstetrics, nephrology, and endocrinology helps balance maternal and fetal risks.
Women with diabetes may face different infection risks and diagnostic pathways. Hematuria, flank pain, and fever still require the same urgency, but imaging choices may shift to minimize fetal exposure. For metabolic inflammation that can influence vascular health, see Metformin and Inflammation for a systems view relevant to long-term kidney protection.
Diagnosis and Monitoring
Evaluation usually starts with ultrasound to confirm fluid content and wall features. When measurements are borderline or features are indeterminate, CT or MRI helps refine classification. Clinicians often document dimensions in millimeters, which guides interval follow-up and helps answer what size of kidney cyst is dangerous in mm based on radiologic criteria and change over time.
Laboratory monitoring includes serum creatinine, eGFR, electrolytes, and urine albumin-to-creatinine ratio. Track blood pressure closely, as hypertension accelerates renal decline. For practical hypertension context in diabetes and CKD, see Atenolol and Hypertension and a beta-blocker overview in Bystolic Blood Pressure Guide. General kidney testing guidance is summarized by national organizations; a concise starting point is the NIDDK resource on kidney health testing (CKD evaluation basics).
Management Options and Referral
Most asymptomatic simple cysts need only periodic imaging. Interventions focus on symptoms, growth, or complex features. Options include percutaneous aspiration with sclerotherapy, cyst decortication, or partial nephrectomy for selected cases. Clinicians individualize follow-up intervals based on cyst class, growth rate, and kidney function trends. Conservative care also emphasizes blood pressure, glycemic targets, and infection prevention.
When symptoms or imaging criteria escalate, urology or nephrology referral is appropriate. Shared care aligns imaging schedules with labs, diabetes medications, and cardiovascular risk reduction. For an overview of renal cysts treatment choices and multidisciplinary coordination, review nephrology-focused content within our site’s categories like Nephrology Products for device and supply context. Diuretic therapy may be used for edema from other renal conditions; see Furosemide Injection for pharmacology details. Diabetes therapies also affect renal outcomes; compare classes in Invokana vs Metformin and explore broader disease topics in the Diabetes Products category.
MODY 5 and HNF1B: Symptoms and Care
HNF1B variants can cause a form of monogenic diabetes often called MODY 5. People may have pancreatic anomalies, low magnesium, gout, or liver enzyme changes alongside kidney findings. Because presentations vary, coordinated evaluation across endocrinology and nephrology is helpful. Genetic counseling supports family planning and clarifies testing options for relatives at risk.
Care plans emphasize kidney preservation, cardiovascular risk reduction, and individualized glucose management. Selecting diabetes therapies accounts for pancreatic reserve, renal function, and hypoglycemia risk. For genetics-focused background in plain language, MedlinePlus Genetics provides an accessible overview of HNF1B-related kidney disease (HNF1B-related kidney disease). This understanding guides when to involve specialists and how to schedule monitoring across organ systems.
Recap
Most renal cysts are incidental and remain stable. Risk rises when complex features, rapid growth, or symptoms appear. Diabetes adds vascular and metabolic stress that can accelerate kidney decline, so blood pressure, glycemic control, and infection prevention matter. A structured imaging approach, routine labs, and timely referrals provide a safe pathway for most people.
Genetic forms such as HNF1B-related disease introduce additional considerations for surveillance and family counseling. Use radiologic categories to structure follow-up, and align medication choices with kidney function. With a steady plan and shared decision-making, patients and clinicians can manage uncertainty while minimizing complications.
Note: Imaging classifications and follow-up intervals evolve as evidence grows; radiology reports should guide specific timing. For incidental cysts and masses, radiology societies publish periodic updates on risk stratification and follow-up frameworks (ACR incidental findings).
This content is for informational purposes only and is not a substitute for professional medical advice.