Clinicians often consider insulin secretagogues when beta-cell function remains adequate. These medicines trigger the pancreas to release more insulin, which can help control post-meal glucose.
Key Takeaways
- Mechanism-focused tools: These drugs stimulate pancreatic insulin release.
- Two main groups: Sulfonylureas and non-sulfonylurea agents (meglitinides).
- Principal risks: Hypoglycemia and weight gain, especially with missed meals.
- Compare options: Sensitizers act differently and may pair with secretagogues.
- Use wisely: Choice depends on goals, comorbidities, and meal patterns.
Insulin Secretagogues: Mechanism, Classes, and Uses
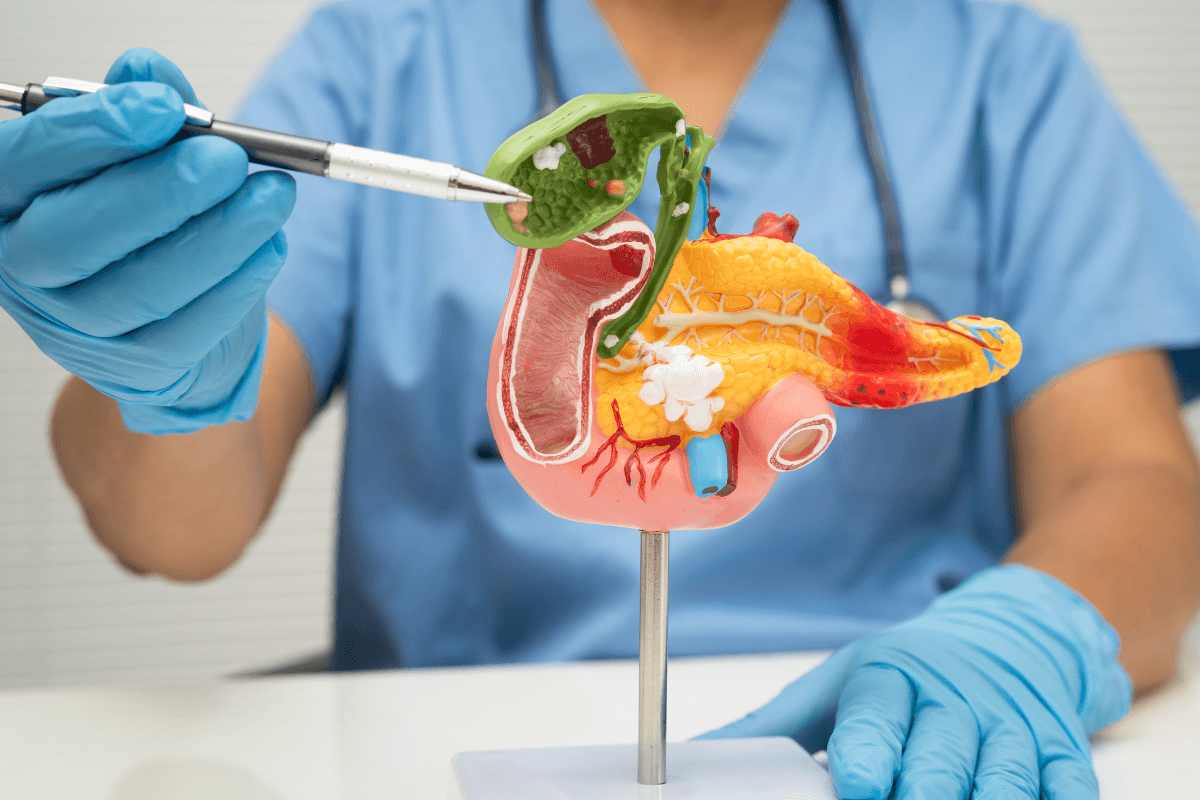
These medicines increase insulin secretion from pancreatic beta cells (islet cells). They close ATP-sensitive potassium channels on beta-cell membranes, which depolarizes the cell and opens calcium channels. Calcium influx then prompts insulin granule release. This pharmacology helps reduce fasting and postprandial glucose, particularly early in type 2 diabetes. However, the effect depends on remaining beta-cell capacity and consistent meal intake.
Secretagogues are not used for type 1 diabetes and are not a substitute for insulin when insulin deficiency is pronounced. Clinical practice guidance describes them as one of several oral options for hyperglycemia management. For broad clinical context, see the NIDDK treatment overview, which outlines medicine classes and goals NIDDK treatment overview. For a concise mechanism overview of sulfonylureas, including potassium-channel effects, consult this clinical reference mechanism overview.
Classification and Examples
Clinically, insulin secretagogues classification groups drugs into two families: sulfonylureas and non-sulfonylurea agents. Both increase insulin release, but they differ in onset, duration, and meal timing flexibility. Sulfonylureas include glipizide, glyburide, gliclazide, and glimepiride. Non-sulfonylurea agents, called meglitinides, include repaglinide and nateglinide. The latter act quickly and have shorter duration, which aligns with mealtime dosing strategies.
Non-Sulfonylurea Options (Meglitinides)
Meglitinides target the same beta-cell pathway but bind at a different receptor site. Their rapid onset and brief action can better match variable eating schedules. This profile may reduce late post-meal hypoglycemia compared with longer-acting agents. For a focused overview of this class, see our primer on Meglitinides Drugs to compare class features and clinical considerations. If you need product specifics, our listings for Repaglinide and Nateglinide outline formulations and practical details for reference.
Insulin Sensitizers vs Secretagogues: Choosing by Physiology
Insulin-sensitizing medicines improve how the body responds to its own insulin rather than increasing secretion. This group includes metformin (a biguanide) and thiazolidinediones (TZDs). Understanding the difference between insulin sensitizers and insulin secretagogues helps align therapy with glucose patterns and comorbidities. Sensitizers may fit when insulin resistance dominates, while secretagogues may fit when post-meal insulin release is insufficient.
TZDs, such as pioglitazone and rosiglitazone, work via PPAR-γ to enhance peripheral glucose uptake. If you want a quick refresher on these agents and their distinctions, our comparison of Actos vs Avandia summarizes class traits for context. For lifestyle strategies that complement drug sensitizers, see Increase Insulin Sensitivity for practical approaches to support insulin action. Many readers also appreciate guidance on how to say technical terms; for example, thiazolidinediones is commonly spoken as “thigh-uh-ZO-li-DIN-dee-owns.”
Common Drugs and How They Work
Among sulfonylurea drugs, glipizide and glimepiride are widely used, while glyburide remains available in some settings. These medicines extend beta-cell insulin release beyond baseline secretion. Timing with meals matters because they can trigger insulin regardless of blood sugar. This mismatch may cause hypoglycemia if food intake is delayed or missed.
Patients often ask what to expect when starting these treatments. For a practical orientation to tolerability and everyday use, see What to Expect on Sulfonylureas, which outlines routine experiences many users report. If you are comparing specific agents, our head-to-heads Glyburide vs Glipizide and Glimepiride vs Metformin discuss differences that clinicians often weigh. For product characteristics, the Glimepiride page lists strengths and packaging to support safe handling.
Benefits and Risks to Know
These agents can meaningfully lower fasting and post-meal glucose for suitable candidates. They are often inexpensive, taken orally, and familiar to many clinicians. That said, insulin secretagogues side effects warrant attention. The chief concerns are hypoglycemia and weight gain, which may be more likely with irregular meal timing or higher doses.
Other adverse effects can include nausea, headache, dizziness, or skin reactions. Rare events such as hyponatremia or hematologic changes have been reported. Drug–drug interactions may increase low-glucose risk, so medication reconciliation is essential. For weight considerations linked to hyperinsulinemia, our overview Insulin and Weight Gain explains mechanisms and monitoring points. Broader pharmacologic context is available in the ADA-aligned materials cited earlier; see the NIDDK resource for balanced summaries NIDDK treatment overview.
Note: Hypoglycemia risk rises when meals are skipped. Carry fast-acting carbohydrate and confirm your plan with a clinician.
Pronunciation and Meaning
In clinical usage, secretagogues meaning refers to substances that promote secretion from glands. In diabetes care, the term typically applies to drugs that stimulate pancreatic insulin release. A practical pronunciation is “seh-KREE-tuh-gogz.” Clear language helps during medication counseling, especially when explaining why timing with meals matters.
Clinicians may encounter varying pronunciations for class names across regions. When discussing TZDs, many say “thigh-uh-ZO-li-DIN-dee-owns.” Clarity avoids confusion when patients read labels or search for education resources. If you prefer a numerically oriented overview of therapeutic options, our Diabetes Medications List provides a concise map of drug families and examples, which can help frame conversations and set expectations.
Natural Sensitizers and Lifestyle Supports
Some people ask about natural insulin sensitizers and other nonprescription supports. Regular physical activity, adequate sleep, and dietary fiber can improve insulin action and post-meal glucose patterns. These strategies complement medicines rather than replace them. Their impact varies by person, baseline fitness, and dietary habits.
Supplements such as cinnamon or berberine are often discussed. Evidence remains mixed, formulations vary, and quality control can differ by product. Discussing these choices with a clinician helps avoid interactions and duplicative effects. For structured, behavior-first options that may enhance drug therapy, see Increase Insulin Sensitivity for practical steps and safety considerations.
Tip: Pair any new routine with glucose monitoring to understand personal response patterns.
Frequently Confused: Metformin and Others
Many readers ask: is metformin an insulin secretagogue? No. Metformin is a biguanide that decreases hepatic glucose output and improves insulin sensitivity. It does not stimulate the pancreas to release insulin. Consequently, it has a lower intrinsic risk of hypoglycemia when used alone compared with secretagogues.
Confusion often arises because both metformin and secretagogues are oral agents used early in type 2 diabetes. Their different mechanisms can make them complementary in selected cases. For a focused discussion on low glucose risk with metformin, see Metformin Hypoglycemia, which explains why episodes are uncommon unless combined with other agents or special circumstances.
Recap
Secretagogues help by boosting pancreatic insulin output, improving fasting and post-meal control in appropriate candidates. Class choice, meal timing, and comorbidities drive suitability. Sensitizers address insulin resistance and can be paired thoughtfully with secretion-based drugs.
Use a stepwise, individualized plan that weighs benefits, risks, and adherence factors. For drug-by-drug context and related comparisons, explore our therapeutic guides, including Diabetes Medications List, which organizes options across classes for orientation.
This content is for informational purposes only and is not a substitute for professional medical advice.