Our pancreas, a silent partner behind the scenes of digestion, also holds the key to keeping our blood sugar in check. But what happens when this unsung hero malfunctions? That’s where the surprising link between pancreatic cancer and diabetes comes in. We’ll uncover how these two conditions can be intertwined and why understanding this connection might be the missing piece for earlier detection and better outcomes.
Understanding Diabetes and Pancreatic Cancer
Diabetes develops when blood sugar levels rise to abnormally high levels. There are two types: Type 1, often found in younger people, where the body attacks its insulin-making cells, and Type 2, more common in adults, often linked to being overweight and not being active.
The typical signs of diabetes include feeling very thirsty, going to the bathroom a lot, losing weight for no reason, feeling tired, and having blurry vision. Doctors check blood sugar levels and use a special test called HbA1c to diagnose it. Managing diabetes early is important to prevent serious problems like heart disease and eye issues.
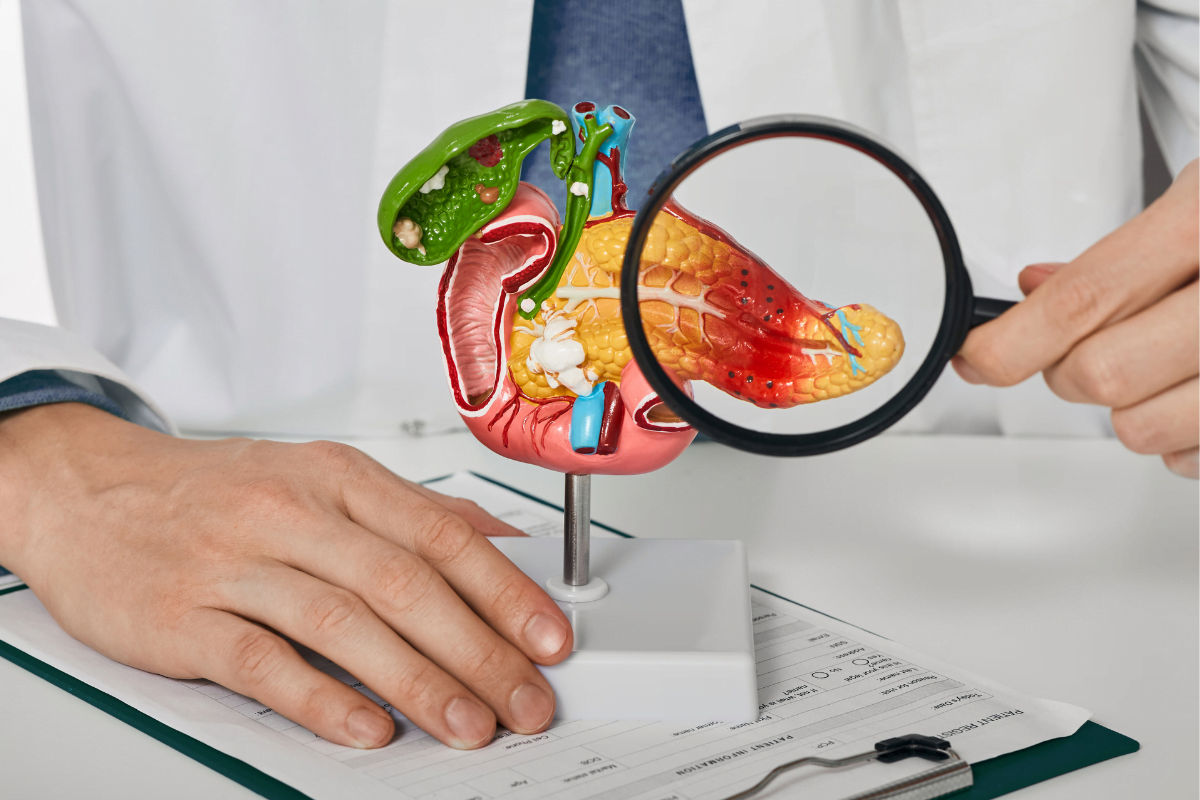
Meanwhile, pancreatic cancer is a serious disease where abnormal cells develop in the pancreas, an organ near the stomach. There are two main types: one starts in the ducts of the pancreas (called adenocarcinoma), and the other in the hormone-producing cells (neuroendocrine tumors).
The risk factors for pancreatic cancer include genetics, meaning it can run in families, as well as certain habits like smoking and being overweight. The condition’s early signs include yellowing of the skin, weight loss, tummy pain, and sometimes new diabetes. Doctors use scans, tissue samples, and blood tests to diagnose it.
The Link Between Pancreatic Cancer and Diabetes
Diabetes and pancreatic cancer share a complex, bidirectional relationship, where each can act as a risk factor for the other. Individuals with long-standing diabetes face an increased risk of developing pancreatic cancer due to prolonged exposure to high levels of insulin and diabetes-related inflammation and metabolic dysregulation, which create an environment conducive to tumor formation within the pancreas.
Conversely, pancreatic cancer can induce diabetes through various mechanisms, including the obstruction of pancreatic ducts, impaired insulin secretion, and disruption of normal pancreatic function, leading to insulin resistance and glucose intolerance.
According to a study documented in Science Direct, diabetes significantly raises the risk of pancreatic cancer, with about half of pancreatic cancer patients also having diabetes. Recent-onset diabetes is closely linked to pancreatic cancer, suggesting it could serve as an early warning sign. The study explores how high blood sugar levels, increased insulin, and insulin resistance may contribute to this heightened risk. Additionally, it discusses the impact of certain diabetes medications, such as metformin, on lowering the risk while highlighting the potential risks associated with other medications.
Furthermore, the study addresses pancreatogenic diabetes, a type induced by pancreatic surgery, and underscores the challenges in managing it. It emphasizes the essential role of diabetologists in the multidisciplinary approach to pancreatic cancer care, focusing on prevention, early detection, and proper management of diabetes in patients at risk for pancreatic cancer.
Prevention and Management
In preventing and managing pancreatic cancer and diabetes, lifestyle modifications play a crucial role. Dietary recommendations are essential, focusing on healthy eating habits, including consuming a balanced diet packed with fruits, various vegetables, whole grains, and lean proteins while limiting processed foods, sugary drinks, and red meat.
Additionally, maintaining an optimal weight through portion control and healthy food choices is emphasized to reduce the risk of both diseases. Physical activity is also vital, with regular exercise helping to control weight, improve insulin sensitivity, and lower the risk of pancreatic cancer and diabetes.
Medical interventions also complement lifestyle modifications in the prevention and management of both conditions. For diabetes management, medications such as metformin are commonly prescribed to regulate blood sugar levels effectively. Potential therapies for pancreatic cancer are being explored, including chemotherapy, radiation therapy, and targeted drug therapies aimed at specific molecular targets.
These medical interventions, combined with lifestyle modifications, form a comprehensive approach to preventing and managing pancreatic cancer and diabetes, improving overall health outcomes for individuals at risk.
Frequently Asked Questions (FAQs)
Can diabetes cause cancer?
While diabetes itself doesn’t directly cause cancer, it heightens the risk of various types, such as pancreatic cancer. Elevated insulin and glucose levels in diabetes can foster inflammation and cell proliferation, contributing to cancer formation.
Does managing diabetes effectively reduce the risk of cancer?
While managing diabetes can help mitigate some of the risk factors linked with cancer, such as controlling blood sugar levels and sustaining a healthy weight, it’s necessary to adopt a comprehensive approach to reduce cancer risk. It includes maintaining a healthy lifestyle, such as regular physical activity, a balanced diet, avoiding smoking, and undergoing recommended cancer screenings based on individual risk factors and guidelines.
Are individuals with diabetes more prone to developing specific types of cancer?
Yes, research indicates that individuals with diabetes have an elevated chance of developing certain types of cancer, including liver, colorectal, breast, bladder, and endometrial cancer. Factors such as insulin resistance, hyperinsulinemia, chronic inflammation, and obesity associated with diabetes may contribute to this increased cancer risk.