Choosing a long-acting basal insulin can shape daily control. This update compares options in plain language and clinical terms. We explain how each works, when they differ, and what to consider during a switch. Early on, we frame Tresiba vs Lantus in practical, day-to-day terms.
Key Takeaways
- Pharmacology basics: different molecules, similar goals.
- Dosing cadence: once daily, distinct flexibility rules.
- Switching safely: plan, monitor, and adjust gradually.
- Hypoglycemia and weight: small but meaningful differences.
- Alternatives: Toujeo, Levemir, and NPH considerations.
Tresiba vs Lantus: Core Differences
Lantus contains insulin glargine U-100, designed for near 24-hour coverage. Tresiba contains insulin degludec U-100 or U-200, formulated for ultra-long action beyond a full day. Both are basal (background) insulins used with or without rapid-acting mealtime insulin.
Pharmacokinetics drive the practical contrasts. Tresiba forms multi-hexamers after injection and releases insulin slowly, supporting once-daily dosing with time-of-day flexibility in adults. Lantus precipitates in the subcutaneous space and dissolves gradually, encouraging a consistent daily schedule. For pharmacology contrasts and context, see Insulin Degludec vs Glargine for a molecule-level overview.
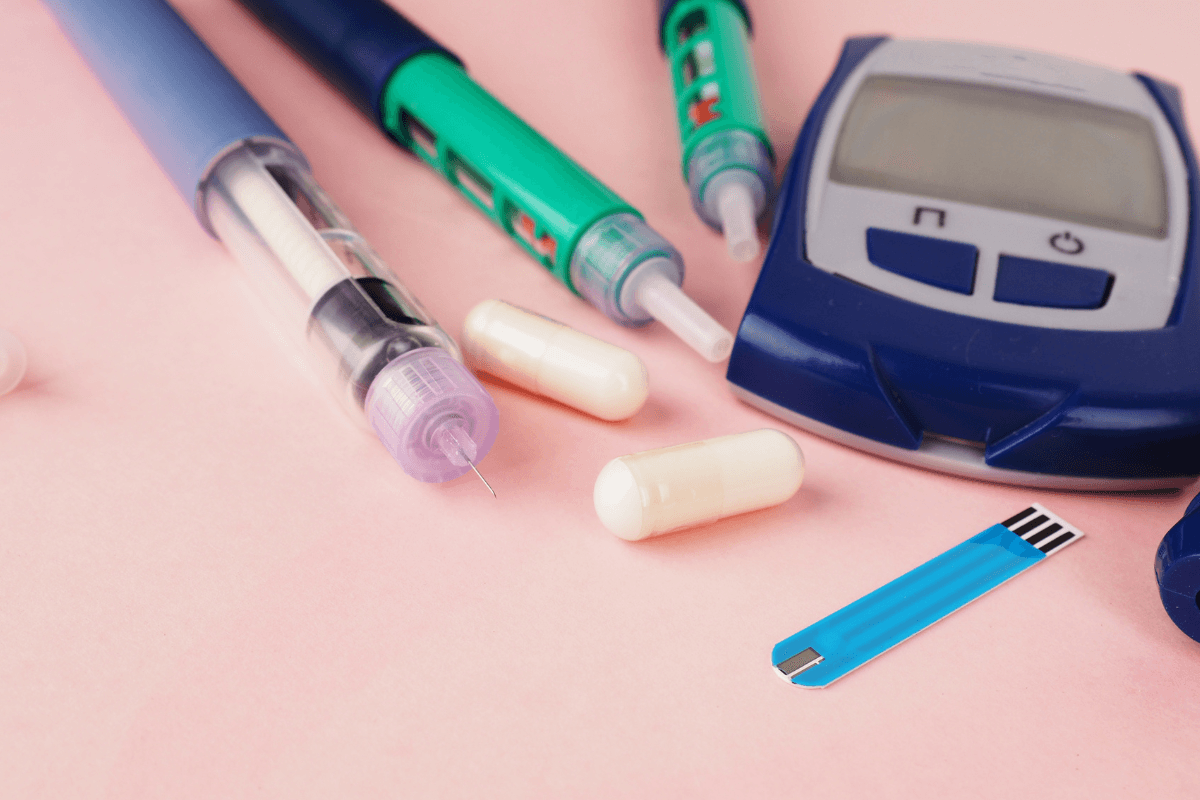
Many patients use pens for convenience. For device formats and strengths, see Tresiba Flextouch Pens. If you prefer glargine pens with a one-dose-a-day routine, see Lantus Solostar Pens for device specifications and strengths.
Evidence-based details about action profiles appear in official labels. The insulin degludec label notes a duration beyond 42 hours and flexible timing in adults, while the insulin glargine label describes near 24-hour coverage and once-daily use at the same time each day. Review the Tresiba prescribing information and the Lantus prescribing information for reference-grade details.
Dosing and Titration in Practice
Daily basal dosing aims to control fasting glucose without excessive lows overnight. In real life, people fine-tune doses over several weeks. Clinicians monitor home readings, A1C trends, and hypoglycemia patterns before adjusting. Those factors often matter more than a single fasting value.
Patterns, not snapshots, guide safe titration. When comparing approaches, clinicians consider tresiba vs lantus dosing, then adjust gradually to avoid nocturnal lows. Pens dose in discrete unit steps; strengths differ, but delivered units are equivalent across pen strengths. For broader regimen context, see Basal vs Bolus Insulin to understand how basal insulin pairs with mealtime doses.
Device details can also influence ease of use. If pen features such as dose memory or tactile feedback matter, review Tresiba Pen Features for handling tips and user-oriented guidance.
Switching Between Basal Insulins
Switching basal insulin should be planned and monitored. Clinicians often start with a conservative unit-to-unit approach, then adjust over several days based on fasting readings and hypoglycemia risk. Steady habits around meals, activity, and sleep help reveal dose needs after a switch.
As a practical matter, tresiba vs lantus conversion depends on prior control, comorbidities, and concurrent therapies. Health professionals may stagger dose changes and use follow-up contacts to avoid overshooting. For background on glargine formulations, see Lantus Vial Guide for formulation specifics and storage considerations.
If you need a refresher on degludec fundamentals before any change, see What Is Tresiba for indications and common precautions. These context pieces help set expectations during transition planning.
Hypoglycemia Considerations
Reducing low blood sugar remains a key goal in basal therapy. Trial data have shown fewer symptomatic and nocturnal events with insulin degludec compared with insulin glargine U-100 in some settings, particularly when titrated to similar fasting targets. Real-world outcomes still vary by individual factors and monitoring habits.
Clinicians weigh tresiba vs lantus hypoglycemia evidence alongside patient history. Monitoring with glucometers or CGM during dose changes can identify early trends. For insight into one product’s adverse effect profile, see Tresiba Side Effects for management strategies. For guideline framing of basal choices and hypoglycemia minimization, consult the ADA Standards of Care for current pharmacologic recommendations.
Weight and Metabolic Effects
Basal insulin can contribute to modest weight gain, largely due to reduced glycosuria and defensive snacking after lows. Comparative data suggest small differences between analogs, but lifestyle factors and hypoglycemia frequency often drive the net effect. Structured nutrition and activity plans help temper unwanted gain.
When considering tresiba vs lantus weight gain, clinicians review past patterns, meal timing, and adjunct therapies like GLP-1 RAs. If weight is a prominent concern, addressing snacks linked to lows may improve both weight and glycemia. Tools like logs or CGM overlays can uncover these patterns efficiently.
Costs and Access
Access and cost-sharing can influence the final choice. Formularies, prior authorization, and device availability vary by plan. Pens and vials may carry different out-of-pocket costs even within the same plan, especially when patient assistance or coupons apply.
Discuss the cost of tresiba vs lantus with your clinician or benefits team to clarify coverage tiers. If glargine alternatives are on formulary, review Basaglar Insulin for a comparable glargine product overview. For a catalog of options, scan Diabetes Products when assessing formats and strengths available in your region.
Related Options: Toujeo and Levemir
Some patients evaluate concentrated glargine or alternative long-acting analogs. Toujeo (insulin glargine U-300) offers a different release profile and may reduce injection volume. In comparative considerations like tresiba vs toujeo, clinicians focus on fasting stability, hypoglycemia patterns, and dosing intervals, rather than headline unit numbers alone.
Other options include detemir (Levemir), which has a shorter duration and may require twice-daily dosing at lower total doses. If considering detemir devices, see Levemir Penfill Cartridges for format specifics. For glargine U-300 background and clinical use, explore What Is Toujeo as you weigh pharmacologic and lifestyle fit.
Interchangeability and Combined Use
At the pharmacy counter, different basal analogs are not automatically substitutable. From a regulatory perspective, pharmacy-level interchangeability applies to specific biosimilar designations, not across distinct molecules like degludec and glargine. Clinical switching is common, but it occurs under prescriber direction with monitoring.
Patients sometimes ask: are lantus and tresiba interchangeable in everyday practice? They can be switched with clinical oversight, but they are not taken together routinely. Overlap strategies may be used briefly during transitions in select cases. If technique is part of the discussion, review Lantus Injection Sites to confirm rotation practices that support consistent absorption.
Timing, Flexibility, and Missed Doses
Time-of-day rules differ between basal analogs. Tresiba allows flexible dosing intervals in adults when at least eight hours separate doses, thanks to its long and flat profile. Lantus performs best with a consistent once-daily time anchored to routine, like bedtime or morning.
Understanding tresiba duration of action helps in planning travel days or irregular schedules. If a dose is missed, labels recommend taking it when remembered and then resuming the usual schedule, while maintaining the minimum interval. For a primer on glargine’s steady activity, see How Lantus Works for mechanism basics. If you want pen-specific handling tips and storage thresholds, see Tresiba Flextouch Pens Guide for practical pen usage details.
Tip: Keep a short written plan for travel, shift work, or illness days. Clear steps reduce missed doses and reactive snacking.
Recap
Lantus and Tresiba both deliver basal coverage, but they differ in duration, flexibility, and some safety outcomes. Choosing between them depends on schedule, hypoglycemia history, and access. When switching, go stepwise and monitor closely. Related options like glargine U-300 or detemir may suit specific needs.
For glargine cartridge handling and steady delivery, see Lantus Cartridge Guide for device-focused pointers. For broader reading across conditions and therapies, browse Diabetes Articles to explore adjacent topics.
This content is for informational purposes only and is not a substitute for professional medical advice.