Getting insulin doses right starts with reading the syringe correctly. Insulin syringe measurement affects how much medicine reaches your body, so small errors can matter. This guide explains markings, unit systems, needle choices, and safe technique in plain terms.
Key Takeaways
- Know your syringe scale and insulin concentration before drawing up.
- Match syringe volume to typical dose to improve accuracy.
- Rotate injection sites to protect skin and absorption.
- Store insulin safely to maintain potency and consistency.
Insulin syringe measurement in Practice
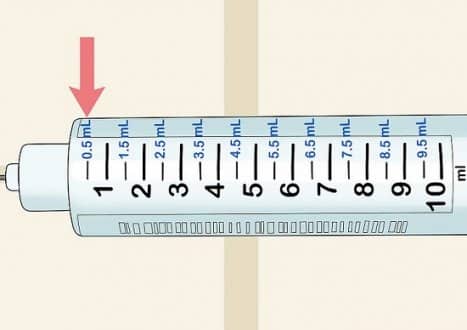
Syringes are calibrated in insulin “units,” not milliliters (mL) alone. With U-100 insulin (100 units per mL), a 1 mL syringe holds 100 units, a 0.5 mL syringe holds 50 units, and a 0.3 mL syringe holds 30 units. The barrel shows major marks (often every 5 or 10 units) and fine tick marks for single units. Knowing which line equals your dose prevents over- or under-dosing.
Choose the smallest syringe that comfortably holds your typical dose. Smaller barrels usually have finer markings, which can help with fractional units and pediatric or sensitive dosing. For example, if you usually take 18 units, a 0.3 mL (30-unit) syringe may offer better readability than a 1 mL barrel. Subcutaneous (under the skin) injections rely on steady technique, consistent angles, and careful measurement to deliver predictable results.
| Syringe Volume | Max Units (U-100) | Common Markings | Typical Use |
|---|---|---|---|
| 0.3 mL | 30 units | 1-unit ticks | Low doses; finer control |
| 0.5 mL | 50 units | 1- or 2-unit ticks | Moderate doses |
| 1.0 mL | 100 units | 2-unit ticks | Higher doses |
Units, Concentrations, and Insulin Conversions
Most vials and cartridges are U-100, but concentrated products exist, including U-200, U-300, and U-500. The unit is constant across concentrations, yet volume per unit changes. Never assume a 1-to-1 swap across concentrations. If a prescriber changes concentration, the dose and delivery device often change too. Safe insulin conversions require explicit instructions from a clinician and the right syringe or pen system to match the product.
Double-check labels, especially when switching brands or formulations. Long-acting analogs and concentrated human insulin follow strict labeling, and their instructions outline compatible devices. For concentration details and precautions, see the Toujeo Dosage Guide for clarity on U-300 handling at Toujeo Dosage Guide. You can also review a long-acting option in the Basaglar Cartridge Guide to understand device-specific dosing steps in practice via Basaglar Cartridge Guide. For background on concentrations and fundamentals, the American Diabetes Association provides a concise overview in its insulin basics resource (ADA insulin basics).
Syringe Sizes, Needles, and Fit
Needles vary by gauge (thickness) and length. Thinner needles (higher gauge numbers) may feel gentler, while length influences the angle needed to stay within the fat layer. Match needle length to your body habitus and technique. Shorter needles can work well for many adults when inserted straight in, but some people benefit from a slight skin pinch to avoid intramuscular delivery.
Pen devices use dedicated tips, and choosing the right Insulin Pen Needles can help limit leakage and improve comfort during injections. If you want more on needle engineering and design options, see the BD Needles Guide for practical selection tips. Syringes and pen tips are single-use items; reuse can blunt tips, increase discomfort, and raise infection risk.
Injection Sites and Technique
Absorption depends on site selection, skin thickness, and local blood flow. The abdomen often provides steady uptake, while the thigh and buttock may be slower. Rotating within a zone reduces lipohypertrophy (lumpy fat) and helps doses act predictably. Many clinicians teach quadrant or grid methods to keep track of rotation without repeating the same spot.
People commonly ask about the How to Use Insulin Pen steps, but injection principles apply to syringes as well: clean hands, check the label, measure carefully, and inject steadily. To protect skin and insulin action, focus on the best insulin injection sites and avoid injecting into scars, moles, or irritated areas. For site maps and technique points, the American Diabetes Association offers practical guidance (ADA injection overview).
When Pens Make Sense: Insulin Pen vs Syringe
Pen devices offer preset increments and reduce certain measurement errors. They also support discreet dosing in public settings. Syringes, however, allow flexible mixing for some regimens and can be more cost-sensitive. Your choice can vary by dexterity, vision, and whether you need fractional-unit dosing beyond what a pen can deliver.
For a direct comparison of features, the editorial breakdown in Insulin Pen vs Syringe explains strengths and trade-offs. If you use a pen platform, this step-by-step NovoPen 4 Guide shows consistent priming and dialing, which translates well to other brands. Device familiarity helps reduce setup errors, prime consistently, and maintain dose accuracy.
Dosing Approaches and Charts
Care teams individualize doses using factors like meals, activity, and fasting patterns. Some plans use a table to adjust doses around food or glucose readings. An Insulin Dosage Chart can illustrate how clinicians adjust amounts safely, but any changes should be guided by your prescriber. Measuring accurately and logging responses helps teams refine doses over time.
Clinicians may use sliding scales or multi-component plans that blend background and mealtime components. Understanding your regimen structure reduces anxiety and improves consistency. For threshold context on hyperglycemia decisions, see When Insulin Is Needed, which explains how providers approach high readings. Bring your logs to appointments so patterns are visible and decisions are data-driven.
Insulin Types and Timing
Different insulin types have distinct onset, peak, and duration patterns. Rapid-acting options cover meals, while basal analogs provide steady background support. Matching your dose timing with meals and activity helps smooth blood glucose changes. Your care team may recommend separating injection timing for different formulations to minimize stacking and variability.
Understanding insulin peak times can help you plan meals and exercise more reliably. For examples, the NovoRapid Cartridge Guide discusses prandial use, while the Basaglar Cartridge Guide outlines basal characteristics. If your plan includes human regular, the same principles of timing and monitoring apply as discussed for concentrated options and rapid analogs.
Storage, Handling, and Safety
Insulin is temperature-sensitive. Keep unopened supplies refrigerated and avoid freezing. Once in use, follow the product’s in-use temperature window and discard date. Confirm label specifics because analogs vary. Learning the recommended insulin storage temperature helps preserve potency and predictable action. Keep vials and pens out of direct heat and sunlight during daily use.
For general supplies, browse the Diabetes Products section to see device accessories commonly used with insulin. For broader handling tips, the American Diabetes Association’s storage guidance details time and temperature thresholds for common products (ADA storage guidance). Keep a written reminder with your kit so you can quickly check time-out-of-fridge limits.
Tip: Photograph your vial label and write the first-use date on a sticker. Visual prompts reduce guesswork when supplies rotate.
Note: If labels or concentrations change, recheck your syringe scale and confirm dosing with your clinician to avoid mix-ups.
This content is for informational purposes only and is not a substitute for professional medical advice.