Diabetes and hypertension are two of the most widespread chronic health conditions affecting adults globally. Together, they build a complex health challenge that can significantly raise the likelihood of heart disease, stroke, and kidney failure. Recognizing the connection between diabetes and hypertension is essential in providing effective, personalized care.
In 2025, healthcare providers are emphasizing preventive strategies and integrative treatments more than ever. With evolving guidelines, innovative therapies, and digital tools, managing these two conditions no longer needs to feel overwhelming. This article explores the best practices for controlling both conditions and improving long-term health outcomes.
Why Hypertension and Diabetes Are Related
Before discussing treatment strategies, it is important to recognize the relationship between these two conditions. They are closely connected and often occur together in what is referred to as metabolic syndrome.
How are diabetes and hypertension linked? When blood sugar levels remain high over time, they damage blood vessels and make them less elastic. This contributes to increased blood pressure. On the other hand, high blood pressure can make it harder for the body to process insulin efficiently.
Both conditions share several risk factors, including:
- Obesity or being overweight
- Lack of physical activity
- Poor dietary habits
- Chronic inflammation
- Insulin resistance
By managing one, patients often see improvements in the other. This overlapping nature is why treatment plans are increasingly coordinated.
Best Practices for Managing Diabetes and Hypertension in 2025
Thanks to new research and tools, managing these two conditions in 2025 is more personalized and technology-driven than ever before. Healthcare professionals now take a more holistic approach that goes beyond medications.
Here are some top strategies being used today:
Lifestyle Adjustments
Lifestyle continues to be the cornerstone of effective management.
- Nutrition: Focus on fiber-rich, low-sodium meals with minimal added sugar. The Dietary Approaches to Stop Hypertension (DASH) diet and Mediterranean diet remain popular choices.
- Physical activity: Aiming for 150 minutes per week of moderate-intensity exercise helps regulate blood sugar and lower blood pressure.
- Weight control: Even modest weight loss can reduce the impact of both conditions.
Medication Management
Treating both conditions often requires a combination of drugs. For diabetes, this may include metformin, GLP-1 receptor agonists, or SGLT2 inhibitors. For hypertension, ACE inhibitors and ARBs are frequently recommended for people with diabetes because of their kidney-protective effects.
Monitoring for side reactions and adjusting doses as needed is critical in maintaining balance between the two.
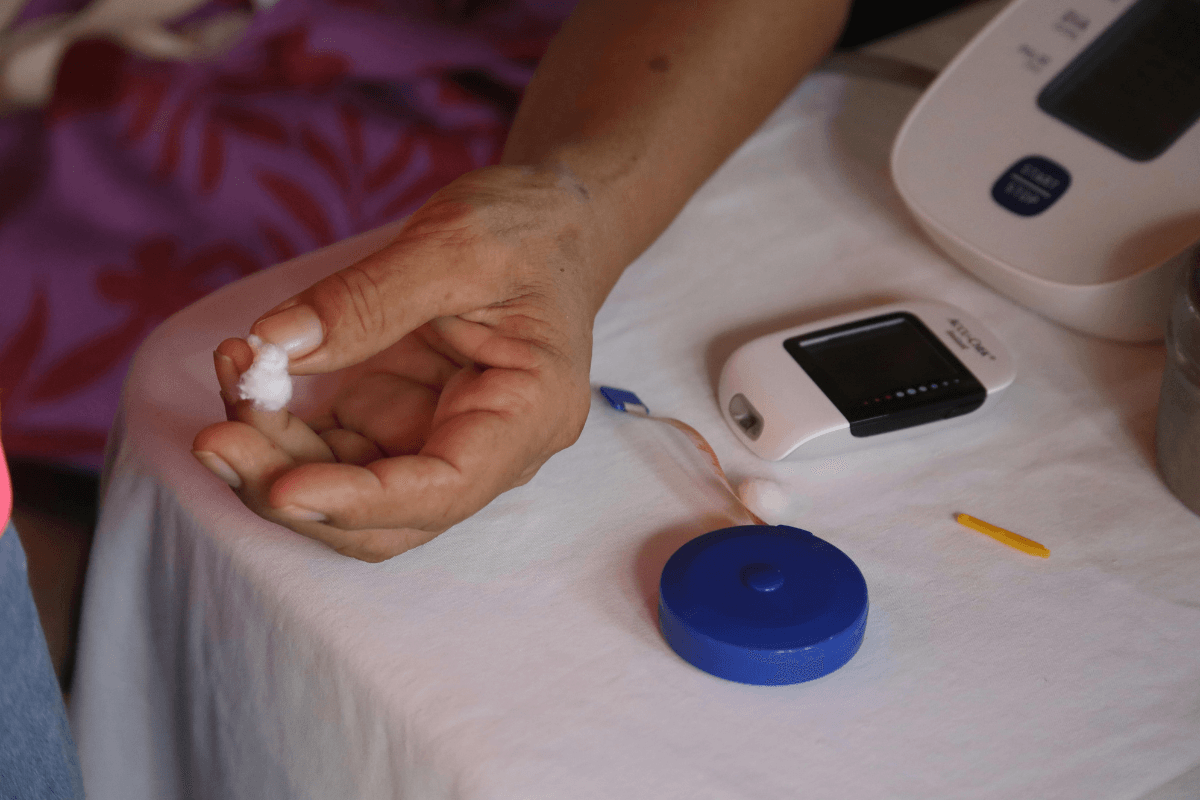
Technology and Digital Tools
Smart devices now make daily monitoring easier.
- Glucose monitors and blood pressure cuffs that sync with apps offer real-time tracking.
- Telemedicine platforms connect patients with their care teams instantly.
- AI-based apps help personalize meal planning and medication reminders.
Team-Based Care
In 2025, many patients will benefit from a team that includes doctors, nurses, dietitians, and health coaches. This collaborative approach ensures that every angle—nutrition, medication, exercise, and emotional health is being addressed.
Setting Realistic Targets
Working with a healthcare provider to set personalized goals is key. These often include:
- Blood glucose (A1C): Target usually under 7 percent
- Blood pressure: Goal often around 130/80 mmHg
- Cholesterol levels: LDL control is essential to reduce cardiovascular risk
- Weight and waist circumference: Even a 5 to 10 percent reduction improves outcomes
Progress should be tracked regularly, and goals should be reassessed during follow-up visits.
Preventing Complications Through Early Action
Even when hypertension and diabetes are present, early detection and intervention can prevent most of the complications. People who adopt good control early have significantly lower chances of:
- Needing dialysis
- Suffering heart attacks
- Losing vision
Routine screening is critical. Patients with either condition should have their blood pressure, A1C, cholesterol, and kidney function checked multiple times per year.
Learn More About Hypertension and Diabetes Medications
If you or a loved one is managing hypertension and diabetes, now is the time to take proactive steps. Schedule a visit with your healthcare provider to review your current medications and consider partnering with a dietitian or health coach to develop a plan tailored to your needs and lifestyle.
With the right support and informed choices, you can take control of your health and boost your quality of life. Explore our selection of diabetes medications and hypertension treatment options—designed to help you manage both conditions effectively and confidently.
Takeaways
The diabetes and hypertension relationship is a critical one. These closely linked conditions, when managed together, can significantly reduce the risk of serious complications. Understanding how they interact helps guide more effective treatment strategies. The best outcomes in 2025 come from combining lifestyle changes, appropriate medications, and smart monitoring tools.
Although the connection between these conditions is complex, early intervention and ongoing support can lead to better overall health and an improved quality of life.
Frequently Asked Questions (FAQS)
Can you manage both diabetes and hypertension with one treatment plan?
Yes, many treatment approaches overlap, especially in terms of diet, exercise, and some medications that benefit both conditions.
Is it common to have diabetes and hypertension at the same time?
Yes. It is estimated that more than 60 percent of people with type 2 diabetes also have high blood pressure.
Are there medications that treat both conditions?
While no single medication treats both completely, some blood pressure medications like ACE inhibitors offer protective benefits for people with diabetes.