Understanding insulin vs glucagon helps explain why blood sugar changes throughout the day. These two pancreatic hormones act in opposite directions to steady glucose. This guide compares their roles, explains clinical basics in plain language, and outlines emergency use of glucagon for severe hypoglycemia. You will also see practical steps for administration, monitoring, and safer follow-up.
Key Takeaways
- Opposite actions: insulin lowers glucose; glucagon raises it.
- Insulin supports storage and use of nutrients after meals.
- Glucagon protects the brain during fasting and lows.
- Emergency glucagon treats severe hypoglycemia when a person cannot self-treat.
- Plan ahead: train helpers, store kits correctly, and monitor afterward.
Insulin vs Glucagon: Core Roles in Blood Sugar
Insulin and glucagon function together like a thermostat. After eating, insulin signals cells to absorb glucose and store energy. Between meals and overnight, glucagon prompts the liver to release glucose to keep the brain supplied. This push–pull balance protects organs from both highs and lows. When the system falters, diabetes therapies and emergency tools help restore stability.
Insulin encourages storage in the liver, muscle, and fat tissue, while glucagon mobilizes fuel when intake is low. The liver responds quickly to both. Skeletal muscle mainly reacts to insulin by taking up glucose for activity and repair. In people with diabetes, therapy aims to reproduce these patterns safely. For a concise hormonal overview, see the NIDDK overview on glucose regulation (NIDDK overview).
Insulin: Structure, Actions, and Everyday Use
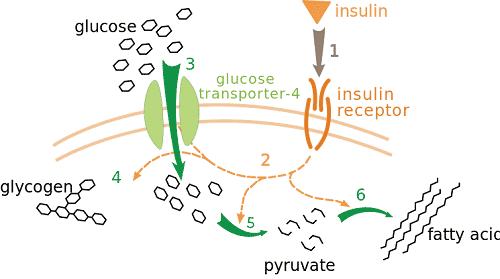
Insulin is a protein hormone made by pancreatic beta cells. It binds to receptors on cells and activates pathways that move glucose transporters to the surface. That action lowers blood glucose and supports energy production. It also promotes glycogen storage in the liver and muscle, and it reduces breakdown of fat and protein.
Clinically, rapid-acting and long-acting formulations help match physiology. Rapid-acting doses cover meals and corrections, while basal insulins smooth the gaps between meals and overnight. To understand therapy timing and absorption, people often learn how does insulin work and how different tissues respond. For an example of rapid-acting therapy in practice, see Humalog Cartridge for mealtime coverage (Humalog Cartridge) and a long-acting option discussed in our Basaglar Cartridge explainer (Basaglar Cartridge).
Mechanism and Tissue Targets
After injection, insulin circulates and binds to insulin receptors (cell-surface proteins). This triggers signaling that moves GLUT4 transporters to cell membranes in muscle and fat. Glucose then enters cells more easily, lowering blood levels. In the liver, insulin encourages glycogen synthesis and limits new glucose production. Muscle uses incoming glucose to refuel glycogen and support activity. Fat tissue reduces lipolysis, which helps limit ketone formation. These effects together steady post-meal rises and maintain energy availability during the day.
Glucagon: Structure, Actions, and Emergency Role
Glucagon is a peptide hormone from pancreatic alpha cells. It raises blood glucose by stimulating glycogen breakdown and new glucose production in the liver. When a person has not eaten or becomes hypoglycemic, glucagon quickly mobilizes glucose to protect the brain. This response is particularly important overnight and during prolonged activity.
Beyond basic glucagon function, emergency formulations are designed for severe lows when a person cannot swallow or self-treat. Traditional kits include a vial of powder and a diluent syringe. Nasal options supply a ready-to-use dose without a needle. For ready-to-use nasal therapy information, see Baqsimi Nasal Powder, which can help in caregiver plans (Baqsimi Nasal Powder). For injectable kits that require mixing, see the Glucagon Injection Kit With Diluent for familiarization and storage needs (Glucagon Injection Kit With Diluent).
When and How to Use Glucagon in Emergencies
Emergency glucagon is intended for severe hypoglycemia with unconsciousness, seizures, or inability to swallow fast sugars. In these situations, a trained helper should give glucagon injection promptly while another person calls emergency services. Do not give food or drink to an unconscious person. Position on the side to reduce aspiration risk, and stay until help arrives.
Community guidelines emphasize preparation and clear steps. Caregivers can practice with trainer devices or review checklists in advance. For a concise step-by-step demonstration with pictures, see our guide on emergency kit technique (Use Glucagon Injection Kit). For formal clinical guidance on treating severe hypoglycemia, review the ADA Standards of Care, which outline treatment thresholds and follow-up (ADA Standards of Care).
Administration Steps for Glucagon
Several formulations exist. Traditional powder kits require mixing the diluent with the vial, drawing up the solution, and injecting into the thigh or arm. Newer products provide ready-to-inject pens or intranasal sprays. Before emergencies occur, check expiration dates and storage limits. Keep kits where support persons can locate them quickly, such as a bag, desk drawer, or gym locker.
Caregivers often ask how is glucagon administered safely under stress. A simple plan helps: assign roles, keep instructions with the kit, and practice reconstitution steps. If the person vomits, maintain side positioning and protect the airway. After successful dosing, glucose usually rises within minutes, but continued monitoring is essential in the next hour. For a needle-free option suitable for some caregivers, consider reviewing nasal glucagon details in the product listing above (Baqsimi Nasal Powder).
Monitoring After Treatment
After any hypoglycemia treatment, recheck glucose at short intervals until levels stabilize. If available, confirm with a meter even when wearing a continuous monitor. People using insulin pumps or recent boluses may need extra observation because active insulin can outlast the initial recovery. Keep a source of fast carbohydrate and a longer-acting snack nearby once the person is alert.
Care teams often discuss when to check blood sugar after insulin injection during sick days or exercise days. Spacing checks helps catch rebound lows once glucagon wears off. A simple meter can support safer decisions during this window; see OneTouch Verio Flex Meter for pairing and logbook features (OneTouch Verio Flex Meter). For accuracy tips, our article on data tracking expands on meter use and context notes (Accurate Glucose Tracking).
Insulin Resistance and Metabolic Context
Insulin resistance means cells respond less to the same insulin signal. The pancreas compensates by producing more insulin, but over time this strain may contribute to hyperglycemia. Weight gain, inactivity, genetics, sleep disruption, and certain medicines can worsen resistance. Addressing these drivers with activity, nutrition, and medical therapy can improve glycemic control and overall cardiometabolic health.
Clinically, teams use diet patterns, exercise programs, and medications to reduce glucose toxicity and improve sensitivity. People often ask what is insulin resistance and how it relates to type 2 diabetes. In some cases, combination agents like Janumet XR may be considered; our product page summarizes formulation factors for discussions with clinicians (Janumet XR). Newer incretin therapies can also reduce glucose burden; see our overview of common drug classes for mechanism summaries (Diabetes Medications Guide).
Common Confusions and Safety Notes
Glucose terminology can be confusing. A frequent mix-up is glucagon vs glycogen. Glycogen is the stored form of glucose in the liver and muscle. Glucagon is the hormone that signals the liver to break down glycogen. Remember: glycogen is storage; glucagon is the hormonal signal. Using simple mental cues can prevent errors during teaching or emergencies.
Glucagon may cause nausea, vomiting, headache, or transient blood pressure changes. These effects typically resolve as glucose normalizes. Read the manufacturer instructions for safety information and contraindications; for example, the FDA glucagon label describes indications, dosing forms, and warnings in detail (FDA glucagon label). For perspective on cardiovascular considerations with incretin therapies, our article on Mounjaro Heart Benefits discusses emerging evidence used in risk–benefit conversations (Mounjaro Heart Benefits).
Practical Tools and Planning
Preparedness reduces risk during lows. Keep a stocked kit with fast sugar, a glucagon device, and a meter. Store dextrose tablets or gel where you spend time. For replenishing fast carbs and reviewing label details, see Dextrose on our catalog, which outlines concentration and portion sizes (Dextrose). If you use pens, confirm your device compatibility and technique before travel or events.
People on intensive insulin therapy may benefit from device checks and refresher training. Having a backup pen can help during pump failures; see NovoPen 4 for durable pen mechanics and cartridge handling tips (NovoPen 4). For broader living strategies, our lifestyle piece offers structured ideas that support safer glucose patterns day to day (Living With Diabetes Tips).
Recap
Insulin lowers glucose by enabling uptake and storage. Glucagon raises glucose by mobilizing liver stores during fasting or severe lows. Plan ahead for emergencies, train helpers, and review your monitoring routine after treatment. For ongoing learning, browse our Diabetes articles to explore related topics and tools (Diabetes Articles and Diabetes Products).
Note: In suspected severe hypoglycemia, activate emergency services and follow local protocols while administering glucagon.
This content is for informational purposes only and is not a substitute for professional medical advice.